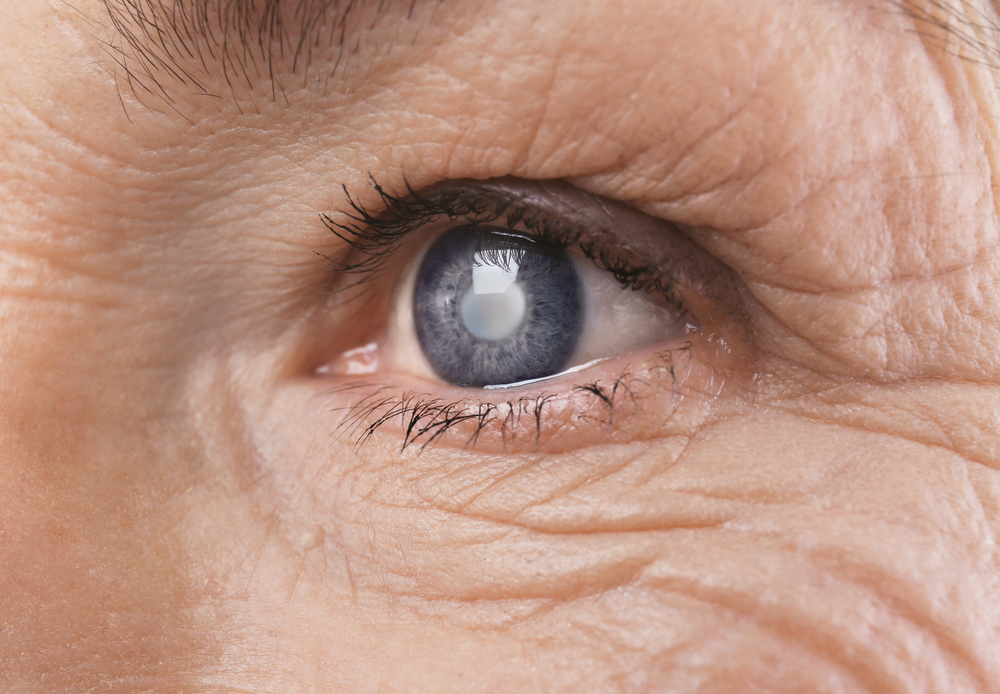
Among the most common causes of blindness in Asia is cataract development, other than glaucoma. Often, around the age of 40, proteins found in the lens of our eyes can start to break down and aggregate. This cluster forms the resulting cloud so characteristic of cataracts, usually developing slowly without setting off any alarm in the early stages.
This cloudiness prevents sufficient light from passing through to the retina, disrupting vision and eventually daily activities such as reading or driving a car during nightfall. Seeing halo-surrounded lights, double vision, and colour-fading are other symptoms faced by cataract sufferers.
What predisposes one to cataracts?
Cataracts are largely associated with age. However, various Asian studies have highlighted a suite of other predisposing factors for this disease, which includes cigarette smoking, diabetes mellitus, excessive UV light exposure, female sex, lower body mass index, and lower socioeconomic status. These factors are on par with studies of Caucasian populations, suggesting common causative mechanisms at play. In younger individuals, cataracts that arise may be congenital, linked to inflammatory eye disease, or due to injury.
Types of cataracts
There are mainly three types of cataracts, each having distinctive characteristics:
- Nuclear sclerotic
- Cortical
- Posterior subcapsular
Nuclear sclerotic
Nuclear sclerotic cataracts are the most prevalently found in patients. It develops very slowly from the inner part of the lens known as the nucleus, eventually moving out to the other layers over time.
With nuclear sclerotic cataracts, individuals often experience an enhancement of near vision. This phenomenon is known as Second Sight. However, this is only temporary and will be succeeded by a deterioration.
Cortical
In contrast to nuclear sclerotic cataracts, cortical cataracts develop from the outside in. Starting at the equatorial cortex and progressing inwards, this type of cataract scatters light travelling to the nucleus. Individuals will find they have trouble with depth perception as a result. Diabetic patients are more likely to develop this variation.
Posterior subcapsular
The symptoms of posterior subcapsular cataracts begin with night vision. The growth begins as a tiny, opaque spot close to the back of the lens. This directly obstructs light, diminishing vision despite a brightly lit environment. Diabetics, individuals with extreme myopia or those that use steroids (whether medically or recreationally) have a higher probability of developing this type of cataract. Posterior subcapsular cataracts develop aggressively, taking months rather than years.
When can you leave them untreated?
Unfortunately, there is no scientifically backed medication to undo or halt the growth of cataracts; they must be removed surgically. This involves the excision of the clouded lens, followed by its substitution with a clear artificial lens.
Until recent technological advancements, cataracts could only be removed at a relatively late phase of development. By then, the cataract would likely have hardened, making extraction difficult. Moreover, when cataracts have been left to progress, loss of vision can occur as a result of glaucoma or inflammation.
At present, it can be removed at any developmental phase.
But the mere presence of a cataract does not warrant going under the knife. They are largely a normal aspect of ageing: many of us would develop cataracts by the time we are 80 as our lens goes through a process of thickening over the years. Near-sightedness because of cataract formation can be alleviated with prescription eyeglasses. The gradual thickening of the lens could simply be rectified by a small yearly change in spectacle prescription.
There are many instances of people living unaffected by them. Lifestyle adjustments can be made in the earlier phases; lights at home can be upgraded or a magnifying glass can be used to aid vision.
When do you need to remove them?
Surgery should only be considered when a disabling glare comes into light; often noticed during driving, activities that require good vision such as playing mah-jong, knitting, watching TV or reading a menu become hard, or when just about any simple task the individual wants to do becomes a challenge. Function is the bottom line here.
On the other hand, there are some cases of people experiencing serious eye problems concurrently with cataracts, such as in macular degeneration with cataracts, or detached retina with cataract. In this case, cataract surgery may not help restore clear vision.
Deciding to go for surgery
If the decision is to go through with cataract surgery, know that a series of tests will need to be performed prior. It is common for medical providers to ensure suitability for surgery by way of blood tests, chest x-rays, electrocardiograms, and ultrasounds. They will also need to assess the required implant strength based on the individual.
Despite all this, the cataract removal procedure tends to be performed on an outpatient basis, i.e. hospitalisation is unlikely. Recovery time is typically short. Depending on the complexity of the cataracts, it could take anything between days to weeks for complete recovery.
Article is written in conjunction with Cataract Awareness Month, which happens in June every year.