Prostatitis is the inflammation or swelling of the prostate gland. It is a common, often painful condition that can happen to men of all ages. However, it is more common for men between 30 and 50 years old. Fortunately, prostatitis can get better with appropriate treatment. Find out more about prostatitis in this article!
PSA: Medical Channel Asia (MCA) is now on Telegram! Join us here for daily reads and the latest updates at your fingertips!
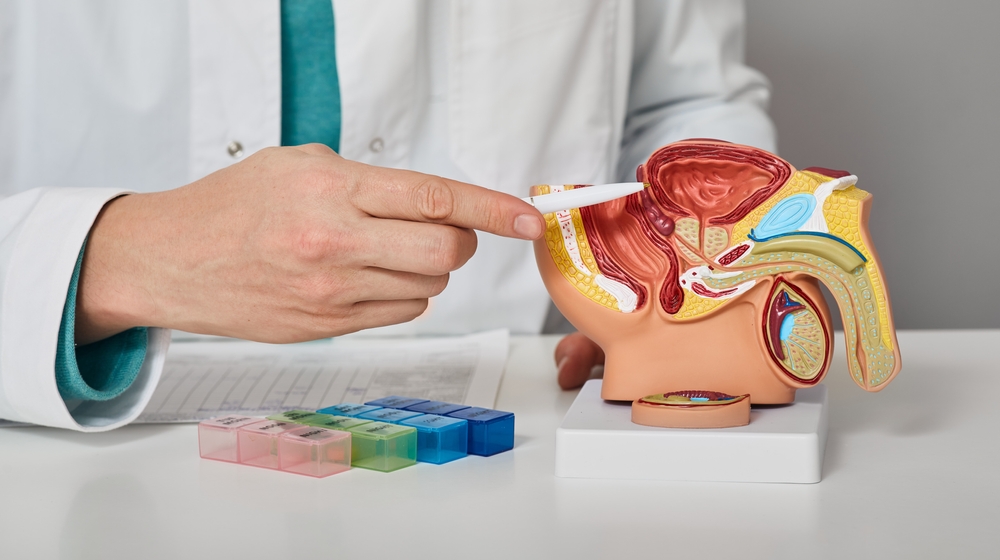
What Is The Prostate?
The prostate is the small gland that sits under your bladder and in front of your rectum. It is responsible for making fluid that provides nutrients for the sperm. The fluid is mixed with the sperm to create semen. The urethra (i.e., the tube that carries urine and semen out of your body) passes through the prostate.

Figure 1: Anatomy of Male Pelvic Area
Symptoms and Causes of Prostatitis
There are 4 types of prostatitis, depending on the symptoms and causes.
1. Chronic Prostatitis
This is the most common type of prostatitis. It can last for months to years, and is considered chronic if your symptoms persist or recur in cycles for at least 3 months. These symptoms may come and go.
Chronic prostatitis is not an infection but an inflammation of the prostate or the nerves around the prostate. Symptoms of chronic prostatitis include trouble and pain when passing urine or during ejaculation. You may also feel pain in the bladder, testicles and penis.
2. Chronic Bacterial Prostatitis
This occurs due to a bacterial infection. Bacteria can get into the prostate when infected urine flows backwards from the urethra. The symptoms onset is slower, and may take longer to treat. Symptoms include a burning feeling when passing urine, increased frequency of urination and pain with ejaculation. Fever or chills are not common.
3. Acute/ Sudden Bacterial Prostatitis
Acute bacterial prostatitis also occurs due to bacterial infection. However, the symptoms can come on quickly. These include fever, chills, very painful burning sensation when passing urine, ejaculatory pain and pain in the pelvis. This type of prostatitis requires immediate treatment.
4. Nonbacterial Prostatitis
In this form of prostatitis, there is no bacteria found in the urine or semen. There is inflammation in the prostate that causes pain. The causes of nonbacterial prostatitis include stress, nerve irritation, injuries or past urinary tract infections.
Risk Factors For Developing Prostatitis
You are more likely to get acute prostatitis if you have:
- Recent urinary tract infection
- Urinary catheter (flexible tube to drain urine from the bladder)
- Prostate biopsy
- Anal sex
- Sexually transmitted infection like HIV or AIDS
- Injured your pelvis
In contrast, you are more likely to have chronic prostatitis if you:
- Are older (men between 50 and 59 years old are 3 times more likely than those between 20 and 39 years old)
- History of prostatitis
- Other medical conditions like irritable bowel syndrome
Diagnosis of Prostatitis
If you have any symptoms mentioned above, you should see a doctor for diagnosis and timely treatment. Your urologist may perform a digital rectal examination to check if there is any swelling or tenderness of your prostate. Your doctor would ask you to lie on your side, with your knees brought up towards your chest. He/she will wear gloves and put some gel on his or her finger before sliding a finger gently into your rectum. It might be slightly uncomfortable but the test is usually not painful and does not take long.

Figure 2: Digital Rectal Examination
Your urologist might also order additional tests for you like urine and blood tests (to see if there is any sign of bacterial infection or any elevated inflammatory markers). Imaging tests (X-ray or ultrasound) might also be done so your doctor can get a view of your urinary tract and prostate to determine the type of prostatitis you have.
Treatment of Prostatitis
Depending on the underlying cause of the prostatitis and the diagnosis, your urologist or doctor would recommend either medications and/or therapy. Most of the time, surgery is not needed.
Antibiotics
If you are diagnosed with a bacterial infection, your doctor would prescribe you with a course of antibiotics. It is important that you complete the course to ensure that the infection clears completely. The duration of antibiotics depends on your condition:
- For acute bacterial prostatitis, you would have to take a 2 to 4 weeks course of oral antibiotics
- For chronic bacterial prostatitis, the course is longer, most often for 4 to 12 week.
If your prostatitis is severe, you might have to go to a hospital for treatment with fluids and intravenous antibiotics (into your veins). Some antibiotics that might be used are trimethoprim-sulfamethoxazole, doxycycline, ciprofloxacin, norfloxacin and ofloxacin.
Other medications
If you are diagnosed with prostatitis not caused by bacteria, your doctor might give you other medications to make you feel better. These medications include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen to reduce pain and inflammation. Some men might find taking a hot soaking bath to be useful to relieve pain. If you have chronic prostatitis related to the nerves, and the pain starts to affect your day-to-day life, you might be prescribed with a medication called gabapentin. Other medications like alpha-blockers (for e.g., tamsulosin) are useful if you have chronic nonbacterial prostatitis. Alpha-blockers relax your prostate and bladder muscles making it easier to urinate.
Extracorporeal Shock Wave Therapy (ESWT)
This is suitable if you have chronic prostatitis without an active infection. The doctor will place a probe over the perineum (which is the space between the scrotum and anus) to deliver shock waves and treat your prostate inflammation.
Conclusion
Prostatitis is common, troublesome and sometimes painful. Fortunately, with appropriate and timely treatment, you would feel better eventually. Moreover, it is important to note that prostatitis does not cause cancer. If you are diagnosed with prostatitis, a marker called the PSA (prostate-specific antigen used to diagnose prostate cancer) might go up. This does not mean you have cancer and you should not be worried. After you have completed treatment for your prostatitis, your doctor would take your PSA again and it would have likely reduced to a normal level.
Did you find this article useful and informative? Do you have more questions regarding this topic, or any other topics related to medical and healthcare? Send your questions to editor@medicalchannelasia.com now!