Testicular torsion happens most commonly between ages 12 and 18. The American Academy of Family Physicians estimated that one in 4000 males younger than 25 years has testicular torsion episodes at least once in their life.
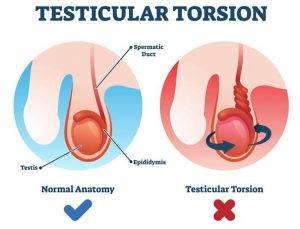
Men have two testicles (testes) each housed in a pouch of skin called the scrotum, located behind the penis. The testes are male reproductive organs which produce sperm and the male hormone testosterone. The spermatic cord carries blood to the testicles. Testicular torsion is a medical emergency where a testicle rotates, twisting the spermatic cord and thereby causing reduced blood flow to the testicle. Without emergency surgery, it can lead to the death of the testicle and associated complications.
A study in Korea concluded that the overall incidence in males was 1.1 per 100,000. However, the incidence in men less than 25 years old was 2.9 per 100,000.
What are the symptoms?
Testicular torsion usually occurs in one testis (unilateral). Symptoms may include:
- Sudden, severe testicular pain which may radiate to the lower abdomen
- Swollen testis; the testis may become larger, red or dark in colour
- Abnormal position of the testis: one testicle positioned higher than the other or at an unusual angle
- Nausea and vomiting
- Frequent urination
- Fever
Other scrotal abnormalities like hydrocele, varicocele, and epididymitis could cause similar symptoms. However, all of them require immediate medical attention.
What Are the Causes?
- Congenital factors/family history of testicular torsion
– Normally, the testicles cannot move freely within the scrotum. In the case of a “bell-clapper” deformity, the testis can move freely in the scrotum due to weak surrounding connective tissue, increasing the risk of the spermatic cord being twisted.
– This genetic predisposition can run in families
- The rapid growth of testicles during puberty
– Testicular torsion commonly affects teens 12 to 18 years old
- Vigorous activity resulting in injury, e.g. sports-related injury to the groin
- Cold climate
– Abrupt temperature changes and contraction of related musculature can cause testicular torsion
- Previous testicular torsion
How is Testicular Torsion Diagnosed?
Besides asking questions to ascertain if your signs and symptoms are caused by testicular torsion, diagnosis may also involve:
- Physical examination of the scrotum, testicles, abdomen and groin.
- Testing of the cremasteric reflex
– The doctor lightly rubs or pinches the inside of the thigh on the affected side. This normally causes the testicle to contract, but the reflex usually does not occur with testicular torsion.
- Tests to rule out alternative causes
– Urine or blood tests to check for infection.
– Scrotal ultrasound to check blood flow. Decreased blood flow to the testicle is a sign of testicular torsion.
– Surgery. Surgery might be necessary to determine whether your symptoms are caused by testicular torsion or another condition.
If pain has been persistent for several hours and the physical examination suggests testicular torsion, sometimes the doctor may just proceed with surgery as any delay may result in loss of the testicle.
What are the treatment options?
Emergency surgery is required in most circumstances once the diagnosis is made. This involves untwisting the spermatic cord to restore blood flow, and testicular anchoring, where one or both testicles are stitched to the inside of the scrotum to prevent free rotation. Ideally, treatment within 6 hours of symptom onset has the best chance of testicular salvage.
People with a known family history of testicular torsion can also choose to have anchoring surgery as a preventative measure.
What are the complications?
If surgery is delayed beyond 6 hours, it could result in tissue death of the affected testicle, possibly requiring surgical removal. This may cause hormonal imbalance, and affect one’s sexual function and fertility.

