A first-of-its-kind calculator may soon change how doctors treat hypertension (high blood pressure), one of the world’s most common chronic conditions.
Researchers built the Blood Pressure Treatment Efficacy Calculator from a meta-analysis published in The Lancet, drawing on data from nearly 500 randomised clinical trials and more than 100,000 participants.
This enables doctors to estimate exactly how much different medications are likely to lower blood pressure – a breakthrough that could help tailor treatment more precisely to each patient’s needs.
Why Blood Pressure Control Matters
“Every 1mmHg reduction in systolic blood pressure lowers your risk of heart attack or stroke by two percent,” explained Dr Nelson Wang, Cardiologist and Research Fellow at The George Institute for Global Health.
The problem, however, lies in complexity. There are dozens of drugs, each available in multiple doses, and most patients need more than one medication to reach safe blood pressure levels. This leaves doctors with thousands of possible combinations and no simple way to predict how effective they will be.
How the Blood Pressure Treatment Efficacy Calculator Work
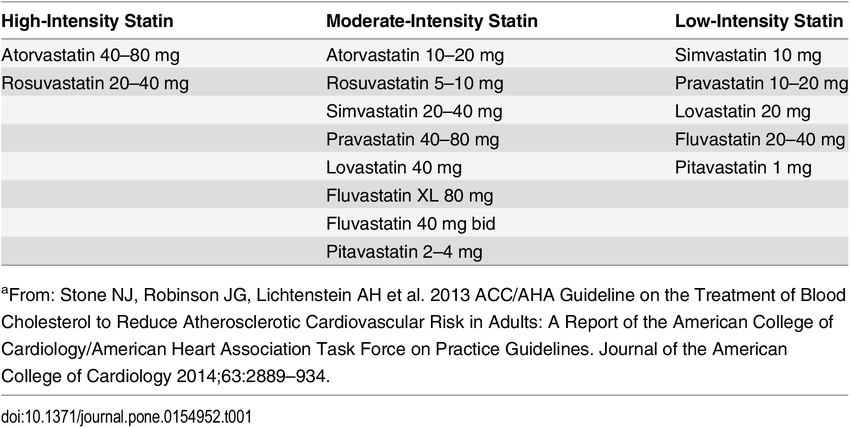
The calculator pools data from hundreds of trials to estimate average drug effects. It then classifies treatments as low, moderate, or high intensity, similar to cholesterol therapy.
Currently, the most common first step is a single antihypertensive medication (monotherapy). But this typically lowers systolic blood pressure by only 8-9 mmHg, while many patients require reductions of 15-30 mmHg.
Traditional approaches, which adjust treatment based on repeated blood pressure readings, often fall short.
“Blood pressure changes from moment to moment, day to day and by season. These fluctuations can be as large as the changes brought about by treatment.”
Dr Wang added, “Measurement practices are also not always perfect, making it very hard to judge how well a medicine is working just by checking blood pressure repeatedly.”
Using the calculator challenges the traditional ‘start low, go slow, measure and judge’ approach.
“With this new method you specify how much you need to lower blood pressure, choose an ideal treatment plan to achieve that based on the evidence, and get the patient started on that ideally sooner rather than later.” Professor Anthony Rodgers elaborated. Professor Rodgers is the Senior Professorial Fellow at The George Institute for Global Health.
Why This Matters
Hypertension affects an estimated 1.3 billion people worldwide and is responsible for around 10 million deaths each year. Called a “silent killer”, it causes no symptoms until it triggers serious complications like heart attack, stroke, or kidney disease. What is alarming is less than one in five people with hypertension have it under control.
The situation is no less serious in Asia. In Singapore, the National Population Health Survey 2022 reported that hypertension affects one in three adults aged 18 to 74. Prevalence has nearly doubled over a decade, rising from about 20% in 2010 to 37.0% in 2022. In Malaysia, the National Health and Morbidity Survey (NHMS) 2019 showed that three in ten adults live with the condition.

Hypertension rates are climbing due to ageing populations, sedentary lifestyles, and diets high in salt and processed foods. Genetic predisposition also matters. South Asian and Malay communities face higher risk, compounded by urban stressors like long working hours.
“Even modest improvements will have a large public health impact,” Professor Rodgers said. “Increasing the percentage of people with controlled blood pressure globally to just 50% could save millions of lives.”
Moving Forward
The next step is to test this approach in clinical trials, where patients can be prescribed treatments according to the degree of blood pressure reduction needed, guided by the calculator.
Western populations still dominate much of the world’s clinical trial data, even though we know Asians may respond differently to certain medications because of genetics, diet, and environment. Researchers can look to to include more local and regional data in trials to ensure the calculator is more relevant for doctors in Singapore, Malaysia, and across Asia.
The Blood Pressure Treatment Efficacy Calculator is now publicly accessible at www.bpmodel.org.
External Reference
- Blood pressure-lowering efficacy of antihypertensive drugs and their combinations: a systematic review and meta-analysis of randomised, double-blind, placebo-controlled trials” by Nelson Wang, Abdul Salam, Rashmi Pant, Amit Kumar, Rupasvi Dhurjati, Faraidoon Haghdoost, Kota Vidyasagar, Prachi Kaistha, Hariprasad Esam, Sonali R Gnanenthiran, Raju Kanukula, Paul K Whelton, Brent Egan, Aletta E Schutte, Kazem Rahimi, Otavio Berwanger and Anthony Rodgers, August 30, 2025, The Lancet. DOI: 10.1016/S0140-6736(25)00991-2
- Hypertension & Heart Health | WHF. (2025). Retrieved from https://world-heart-federation.org/what-we-do/hypertension/
- Stone, N. J., Robinson, J. G., Lichtenstein, A. H., Bairey Merz, C. N., Blum, C. B., Eckel, R. H., Goldberg, A. C., Gordon, D., Levy, D., Lloyd-Jones, D. M., McBride, P., Schwartz, J. S., Shero, S. T., Smith, S. C., Jr, Watson, K., Wilson, P. W., & American College of Cardiology/American Heart Association Task Force on Practice Guidelines (2014). 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology, 63(25 Pt B), 2889–2934. https://doi.org/10.1016/j.jacc.2013.11.002

