In a groundbreaking move, the Asia-Pacific region has introduced its first set of guidelines dedicated to managing X-Linked Hypophosphatemia (XLH), a rare genetic disorder affecting bone growth.
The consensus, spearheaded by an expert panel and endorsed by numerous societies, offers hope for better care. A core expert panel recently formulated the first evidence-based recommendations to optimise and standardise XLH care across the APAC region. The panel comprised 15 pediatric and adult endocrinologists from nine Asia-Pacific (APAC) countries. The Journal of Bone and Mineral Research has published these recommendations.
Learn More About X-Linked Hypophosphatemia (XLH)?
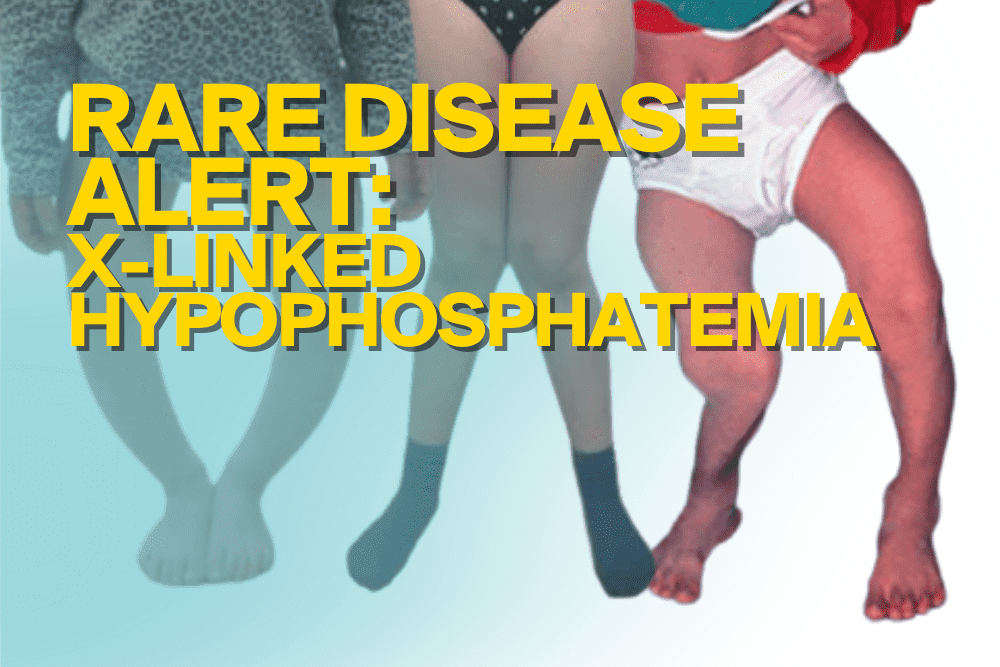
X-linked hypophosphatemia (XLH) is a rare, inherited multisystem disorder that alters bone mineral metabolism.
Dr Manju Chandran is Senior Consultant and Director of Osteoporosis and Bone Metabolism Unit, Department of Endocrinology, Singapore General Hospital. He is one of the authors of the guidelines. Dr. Manju states that the loss of the mineral Phosphate through urine causes XLH. He explains that this leads to ‘poorly mineralised bones and teeth, resulting in short stature, severe bone and tooth fragility, fractures, hearing loss, tooth abscesses, musculoskeletal abnormalities such as joint stiffness, severe bone and joint pain, inability to walk etc. Life span is shortened considerably because patients may develop complications such as kidney failure.’
Misdiagnosis: A Prevailing Issue
XLH affects about 1 in 20,000 people. Dr Craig Munns, Mayne Professor of Paediatrics and Director, Child Health Research Centre, South Brisbane, Queensland, Australia, explains that XLH is often misdiagnosed. He stated, “Unfortunately, XLH is often misdiagnosed for the more prevalent nutritional rickets associated with Vitamin D deficiency, which like XLH, may present with bone pain and insufficiency fractures in adults, and bowing deformities of the lower extremities in children”
Regional Approach to Treatment
The necessity for an Asia-Pacific-centric approach was due to significant variations in regional population genetics and resource availability. Therefore, this tailored set of recommendations fills a critical gap. They provide guidance for healthcare professionals across the diverse landscape of APAC. Local and regional endocrine and research societies, along with patient advocacy groups, have rallied in support of these guidelines. They believe this consensus will be instrumental in enhancing the standard of care for individuals with XLH.
Dr Munns explained, “All the previous X-Linked Hypophosphatemia (XLH) treatment guidelines had been developed from the Western experience of diagnosing and treating the rare genetic disorder. However, regional differences in the population makeup and availability of resources meant these were not always relevant, so there was a need for guideline treatment recommendations tailored to the APAC context, and that is what inspired the panel to develop the new consensus recommendations.”
Dr Munns added that “the recommendations we settled on 16 consensus statements addressing the screening and diagnosis, multidisciplinary management, and transition of care of XLH from childhood to adulthood. Ultimately, optimised care for XLH patients requires prompt identification and early diagnosis; timely multidisciplinary care with regular monitoring and follow-up; and a seamless transfer of care from paediatrics to adult services through the coordinated effort of all stakeholders. Based on the best available evidence, we outlined specific guidance for clinical practice in APAC settings.”
XLH: A Lifelong Journey
XLH, resulting from PHEX gene mutations, impacts not just bones but also dental health and can lead to long-term disabilities. Consequently, the importance of a seamless transition in care from childhood to adulthood is emphasised to cater to evolving healthcare needs across different life stages.
The guidelines also targets to ensure earlier detection and management of the condition from a young age. Dr Manju added that ‘Many a time, this transition of care is poor and the adult patient falls off the treatment bandwagon resulting in very many complications some of them irreversible such as severe musculoskeletal problems including gait abnormalities, kidney failure etc.’’
A Step Forward in XLH Management
The expert group is optimistic that this consensus will guide physicians in delivering consistent and optimal care. Additionally, this will establish a previously absent clinical practice standard in many APAC regions.
Dr Manju hopes that “the guidelines will benefit both health care professionals and patients, by providing clear, pragmatic, real-world evidence-based recommendations for the diagnosis, assessment, treatment and monitoring of patients affected with the disorder.”
Finally, The Journal of Bone and Mineral Research has made this vital document available to all.