Epididymitis is an inflammation of the tube (epididymis) at the back of the testes that stores and carries sperm. Sperm start growing in the testes and gain movement and maturity while travelling through the epididymis. If the testes are also inflamed, this condition is known as epididymo-orchitis.
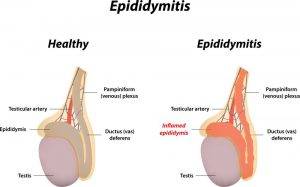
Figure 1: Epididymitis
Symptoms of Epididymitis
If you have epididymitis, your scrotum (the bag of skin containing your testes) might feel tender, warm and swollen. This is the main symptom. There could also be sudden or gradual pain in one or both of your testes. The pain usually starts at the back of one testis and soon spreads to the whole testis, scrotum and sometimes your groin. The whole scrotum can also swell up with fluid (due to the build-up of fluid around your testis), forming a hydrocele. Depending on the cause of the inflammation, you could also experience difficulty in urination or white, yellow or green discharge from the tip of your penis.
Types and Causes of Epididymitis
-
Acute Epididymitis
Acute Epididymitis is when the pain, swelling and inflammation of the epididymis lasts less than 6 weeks. Acute epididymitis can be caused by the following factors:
- Bacterial infection: Most commonly the bacteria is E. coli. The source of infection could be from the urethra (urethritis), bladder (cystitis), prostate (prostatitis) or kidney (pyelonephritis) and then spreads to the testis.
- Sexually transmitted disease (STD): This is more likely in men under 35 years old. The causative bacteria is mostly chlamydia or mycoplasma and rarely gonorrhoea.
- Enlarged prostate blocking the bladder
- Partly blocked urethra (the tube that carries urine and semen out of your body)
- Recent catheter use
- Non-bacterial causes: Urine flowing back to the epididymis, causing swelling but no infection. This usually happens in people who do the heavy lifting.
- Medication use: Rarely medications, for example, amiodarone, can cause epididymitis.
-
Chronic Epididymitis
Chronic Epididymitis is characterised by 6 or more weeks of symptoms, including discomfort or pain in the scrotum, testis or epididymis. Chronic infectious epididymitis is commonly caused by mycobacterium tuberculosis (TB) and should be suspected especially if you have a known history or recent exposure to TB. A chronic case may also result after acute epididymitis that does not seem to go away. Sometimes, the cause cannot be determined, especially if there are no acute symptoms or known infection.
Diagnosis of Epididymitis
If you have any of the above symptoms, it is important to see your doctor to find out the cause of your symptoms. Your doctor would run some tests such as groin examination, urine and blood tests or rectal examination (to rule out prostatitis). Urine bacterial cultures would also be performed to evaluate if there is any bacterial infection in the genitourinary system and determine what type of antibiotics are able to kill the bacteria. If the pain onset is quick and severe, your doctor might do an ultrasound to look more closely at your testes. Ultrasound is used primarily to rule out other causes of pain, like torsion of the spermatic cord, which is a surgical emergency.
Treatment of Epididymitis
The goal of treatment would be to cure any bacterial infections and improve the symptoms. If applicable, the treatment also aims to prevent complications and transmission of sexually transmitted diseases. Most men can be treated at home and do not require hospitalisation. Only when the symptoms are severe, for those with high fever and vomiting (unable to take oral medications) or in older patients, hospitalisation might be considered.
-
Antibiotics
Treatment often starts with a 10 days course of antibiotics. Some examples include doxycycline or levofloxacin. The antibiotics might be changed based on the bacteria that is found in your urine culture. Your symptoms should improve after 3 days of taking antibiotics. However, it might take 2 weeks to months for the discomfort and swelling to ease completely. If your symptoms do not improve after 3 days of treatment or even worse, do consult your doctor again.
-
Anti-inflammatory medications
Your doctor might also prescribe you medications to help reduce the pain and swelling. Some examples include ibuprofen or naproxen.
-
Bed Rest and Scrotal Elevation
Other than medications, if you are diagnosed with epididymitis, you should rest for 1 to 2 days with the scrotum raised if possible. Getting the inflamed area above the level of the heart helps increase blood flow, reduces swelling and speeds up healing. You can also place a cold pack on your groin to ease the pain and swelling.
-
Surgery
In rare cases, if all else fails, your doctor might suggest removing the epididymis. This surgery is known as “epididymectomy”. In this surgery, the testis can be left intact. After surgery, most men would feel better after a few weeks of healing.
-
Management of Sex Partners
If your epididymitis is confirmed to be caused by gonorrhoea or chlamydia, do refer all sex partners during the 60 days before the start of your symptoms to a doctor for evaluation and testing. If the last sexual intercourse was more than 60 days before the start of your symptoms or diagnosis, the most recent sex partner should see a doctor for evaluation and testing.
Conclusion
Epididymitis represents a common medical condition in urological outpatient clinics. Most of the time, epididymitis is caused by bacterial infection. However, there may be other causes as discussed above. If you have symptoms such as pain and swelling in the testis, scrotum or groin, it is important to see your doctor for evaluation. Do not try to self-treat or delay treatment.

