The Embodiment of Trauma: Unravelling the Threads of Science
Where does trauma hide? Is it only a mental phenomenon, or can it insidiously slip into the very tissues of our bodies? This article delves into the intriguing evidence-based enquiry on whether trauma is stored in the body.
The Roots of Trauma: A Psychological Perspective
Trauma, from a psychological perspective, is a complex and multifaceted concept that has been studied extensively. The American Psychological Association (APA) categorizes trauma as an emotional reaction to a distressing or life-threatening event.
Events of this nature can vary widely, ranging from personal occurrences like accidents or physical abuse to large-scale situations such as war or natural disasters.
Furthermore, chronic stress and ongoing exposure to traumatic incidents can have particularly detrimental effects on individuals, especially those living in areas plagued by conflict. In such cases, individuals may experience sustained traumatic stress, which is also known as complex trauma. Unlike single-incident trauma, this form of trauma involves repeated or prolonged exposure to highly stressful events.
The Brain’s Unique Processing of Distressing Memories
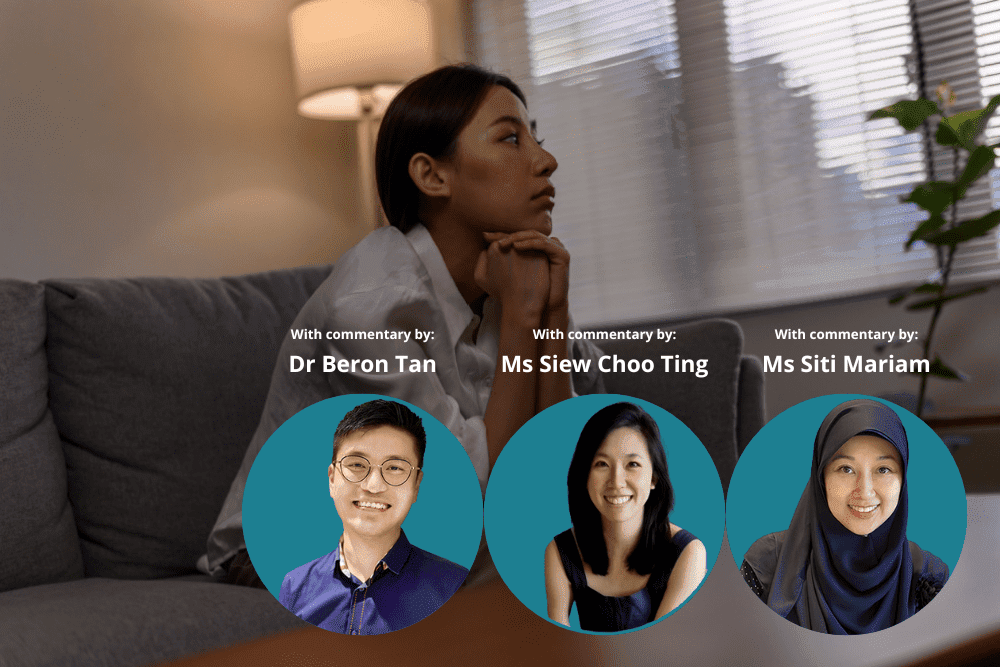
Dr. Beron Tan, a Senior Psychologist who works with children and adolescents at Private Space Medical, provides further insight into how the brain perceives traumatic events.
“When a traumatic event occurs,” he explains, “the memory is perceived by the brain as atypical. It doesn’t get processed in the same manner as typical memories by the hippocampus, the brain’s memory processing centre.” This deviation in processing means that the sensations, images, feelings, and thoughts linked with the traumatic event are fragmented, and lack a defined “timestamp”.
“As a consequence,” Dr. Beron continues, “individuals might experience the traumatic memory as if it were occurring in the present moment, and on an ongoing basis.” Their bodies remain on high alert, attempting to guard against what it perceives as a continuous threat. When exposed to stimuli that remind them of the traumatic event, such as particular smells, thoughts, sounds, or words, they could be overwhelmed with panic symptoms. This includes reactions like hyperventilation, heart palpitations, light-headedness, intense fear, tremors, and even fragmented memory flashbacks.
“These reactions can be so unsettling,” Dr. Beron notes, “that many start to avoid environments that could trigger these feelings. And because these triggers often operate outside conscious awareness, many don’t even understand what’s causing their distress.” This might lead them to adopt a broad safety approach, isolating themselves from potential triggers. Activities like taking public transport, dining in public, or attending work or school could become daunting endeavours they opt to avoid.
Trauma: Beyond the Mind
Although the psychological impacts of trauma are well-known, an emerging body of research suggests that trauma can be embodied. Specifically, embodied trauma refers to the physiological changes that can occur within a person’s body as a direct result of a traumatic event.
Moreover, trauma can manifest physically through significant alterations in the autonomic nervous system (ANS), which, in turn, impacts various bodily functions. These may include changes in heart rate, digestion, respiratory rate, and even gland function. This growing understanding of the connection between psychological and physiological responses to trauma opens new avenues for comprehensive treatment approaches.
Physical Manifestations of Embodied Trauma
Research has shown that the bodily expressions of trauma can be wide-ranging and encompass a variety of symptoms. For instance:
- One significant manifestation of trauma is chronic pain. Trauma survivors often report experiencing unexplained chronic pain, which can be attributed to the body’s stress response system becoming persistently activated. This, in turn, leads to increased muscle tension and pain.
- Additionally, trauma can also impact the gut-brain axis, a well-documented connection between the mind and the gut. As a result, individuals may experience gastrointestinal problems, such as irritable bowel syndrome (IBS) or other digestive issues.
- Furthermore, cardiovascular issues can arise due to changes in the ANS resulting from trauma. These changes can impact heart rate and potentially increase the risk of cardiovascular diseases, including hypertension and heart disease.
- Moreover, the immune system can become dysregulated in response to the persistent stress from trauma. This dysregulation can lead to an imbalance in the immune system, making individuals more vulnerable to infections and autoimmune diseases.
Building on this, Ms. Siew Choo Ting, Principal psychologist who works with youth and adults at Private Space Medical, adds:
“Trauma disrupts the body’s nervous system and natural regulatory processes. When a person experiences trauma, the body’s natural fight, flight, or freeze responses can become overwhelmed, leaving the nervous system stuck in a state of hyper- or hypoarousal. Hyperarousal can exacerbate symptoms such as chronic pain, muscle tension, and hypersensitivity to stimuli, while hypoarousal might lead to persistent low energy, exhaustion, digestive problems, and a weakened immune function. Additionally, there may be noticeable alterations in brain function, including poor memory and emotion dysregulation. These physiological disruptions further emphasise the intricate connection between the mind and body in response to trauma.”
Therapeutic Interventions for Embodied Trauma
As we advance in our understanding of the multifaceted impacts of trauma, recognizing its embodiment is crucial. Consequently, therapeutic interventions are evolving to address both psychological and physiological aspects of trauma.
Here are a couple of noteworthy approaches:
- Somatic Experiencing (SE): This therapeutic approach places the body at the forefront of trauma healing. Developed by Peter Levine, SE encourages the release of trauma stored in the body through sensation-focused therapeutic exercises.
- Eye Movement Desensitisation and Reprocessing (EMDR): Created by Francine Shapiro, EMDR incorporates eye movements or other left-right stimulation to assist in the processing and resolution of traumatic memories. This approach aims to reduce the intensity of emotionally charged memories of traumatic events.
The Body’s Response to Trauma: Insights from Therapist
Further, emphasising the body’s responses to trauma, Ms. Siti Mariam, Principle Therapist specialising in grief and trauma at Private Space Medical, shares:
“When the body experiences serious threats in the form of trauma, it takes action to protect itself. Fight, flight, and freeze are 3 common responses. Fight responses include screaming, crying, or aggression. Flight responses encompass avoidance, escaping, or distracting oneself with other activities. Freeze responses are characterized by feeling numb, sleeping more, reduced heart rate, and being ‘lost for words’. While these responses may offer short-term relief and typically reduce in intensity over time, it’s essential to help the body return to a state of calm and safety.
To assist in this process, practical skills can be applied. Breathing slowly and deeply, retreating to a calm and quiet space, ensuring adequate rest, exercising, eating well, speaking with a trusted individual, or cuddling with a pet can all be beneficial. If traumatic memories or triggers persist, causing distress and impacting daily life, it may be crucial to consider seeking professional help.”
The Winding Path Ahead
While we’ve made significant strides in understanding the embodiment of trauma, it remains a complex and multifaceted issue. Moreover, as more evidence surfaces, it will likely reshape our views on trauma, its impact, and its treatment. For those bearing the invisible scars of trauma, this emerging knowledge could herald a more holistic and effective approach to healing.
References
- Substance Abuse Treatment (US), C. F. (2014, January 1). Understanding the Impact of Trauma – Trauma-Informed Care in Behavioral Health Services – NCBI Bookshelf. Understanding the Impact of Trauma – Trauma-Informed Care in Behavioral Health Services – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK207191/
- Is traumatic stress research global? A bibliometric analysis – PubMed. (2014, February 20). PubMed. https://doi.org/10.3402/ejpt.v5.23269
- Jia, X., Ying, L., Zhou, X., Wu, X., & Lin, C. (2015, March 27). The Effects of Extraversion, Social Support on the Posttraumatic Stress Disorder and Posttraumatic Growth of Adolescent Survivors of the Wenchuan Earthquake. PubMed Central (PMC). https://doi.org/10.1371/journal.pone.0121480
- Psychological stress and disease – PubMed. (2007, October 10). PubMed. https://doi.org/10.1001/jama.298.14.1685
- Hypertension in relation to posttraumatic stress disorder and depression in the US National Comorbidity Survey – PubMed. (n.d.). PubMed. https://doi.org/10.3200/BMED.34.4.125-132
- The role of corticosteroids and stress in chronic pain conditions – PubMed. (2010, October 1). PubMed. https://doi.org/10.1016/j.metabol.2010.07.012
- Shapiro, Francine & Solomon, R.M.. (2010). Eye Movement Desensitization and Reprocessing. 10.1002/9780470479216.corpsy0337.