Prostate cancer treatment has advanced significantly over the years, with surgery and radiation therapy emerging as the most common options for localised disease. Prostatectomy, whether performed through open surgery or robotic-assisted techniques, has long been considered a standard of care. Meanwhile, stereotactic body radiotherapy (SBRT) has gained prominence as a non-invasive alternative that delivers highly focused radiation over a shorter time frame.
Both options offer excellent cancer control, but their differences in invasiveness, recovery, and impact on quality of life are critical factors in deciding the best approach.
Prostatectomy: The Traditional Standard

Prostatectomy involves physically removing the prostate gland, which can be reassuring to patients who prefer an immediate and tangible solution. By eliminating the tumor entirely, surgery often provides peace of mind. The post-operative tissue can be thoroughly examined to determine the precise stage and grade of the cancer. These findings can guide further treatment if necessary.
Risks & Complications
However, prostatectomy is a major procedure requiring general anaesthesia, hospitalisation, and weeks to months of recovery. While robotic-assisted surgery has reduced incision size and improved precision, the risks remain significant. Common complications include bleeding, infection, and the potential for blood clots.
Beyond the immediate risks of surgery, many men face long-term challenges after prostatectomy. Urinary incontinence is a frequent outcome, as the procedure often disrupts the sphincter muscles that control urine flow. This can leave patients reliant on adult diapers (“pampers”) for weeks or even months post-surgery. For some, this situation may persist indefinitely.
Additionally, prostatectomy carries a notable risk of erectile dysfunction due to nerve damage during the operation, which may not fully resolve even with time or medication. The psychological impact of these side effects can be profound, affecting self-esteem, intimacy, and overall quality of life.
Stereotactic Body Radiotherapy (SBRT): An Alternative
In contrast, SBRT is a cutting-edge radiation therapy that treats prostate cancer with precision-guided, high-dose radiation over just five sessions, typically completed within one to two weeks.
Key Advantages of SBRT
Unlike surgery, SBRT is non-invasive, requiring no incisions, anaesthesia, or hospital stays. Patients can return to their normal activities almost immediately after each session, which is particularly appealing for those with busy schedules or a preference for minimal disruption to daily life.
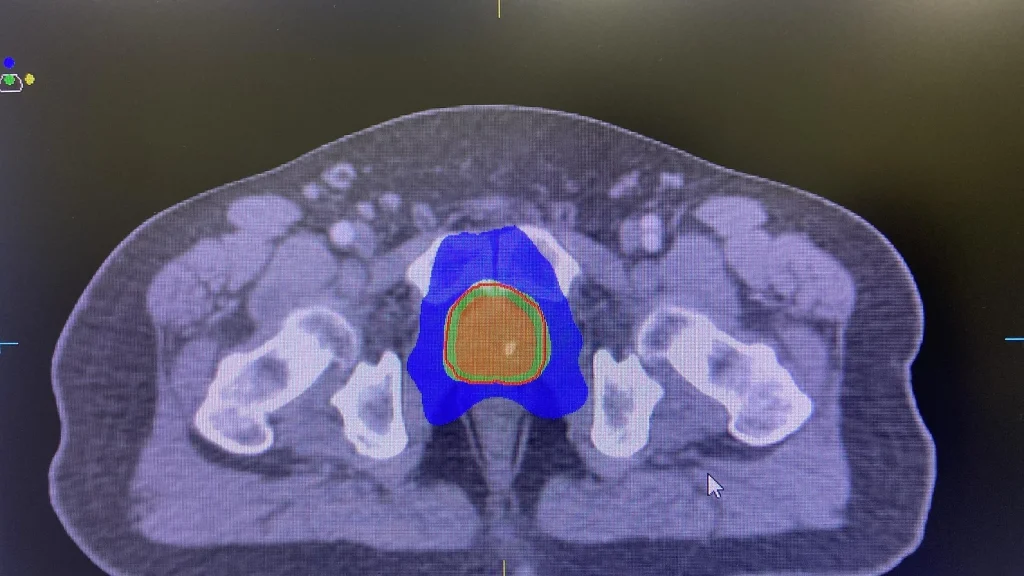
A key advantage of SBRT is its accuracy, which is enhanced by advanced imaging techniques. These include MRI fusion and the use of fiducial markers, or “prostate seeds“. These small markers are implanted into the prostate before treatment to help guide the radiation beams with millimeter precision.
To further minimize the risk of side effects, many centers now use biodegradable spacers like Barrigel, which create a protective barrier between the prostate and rectum. This reduces radiation exposure to surrounding tissues and lowers the chances of bowel complications.
The benefits of SBRT extend beyond its convenience and precision. Studies have shown that SBRT provides cancer control rates comparable to those of surgery for low- and intermediate-risk prostate cancer.
Moreover, SBRT is associated with a lower risk of urinary incontinence and erectile dysfunction compared to prostatectomy.
While some patients may experience temporary side effects such as urinary frequency, rectal irritation, or mild fatigue, these symptoms typically resolve within weeks, leaving most men with a preserved quality of life.
Comparing Prostatectomy and SBRT
For some men, the gradual decline in PSA levels following SBRT, as opposed to the immediate drop seen with surgery, may be a concern. This is often offset by the long-term benefits of SBRT, such as fewer disruptions to daily living and less risk of post-treatment complications.
Importantly, SBRT also accommodates older patients or those with co-existing health conditions who may not be able to withstand the physical toll of surgery. The minimally invasive nature of SBRT ensures that effective cancer control can be achieved without unnecessary risks.
The post-treatment experience also varies greatly between SBRT and surgery. While men recovering from prostatectomy often need to adjust to the reality of wearing diapers and dealing with surgical recovery, SBRT patients can resume their usual routines almost immediately. This not only preserves physical independence but also alleviates the psychological strain often associated with invasive procedures.
Looking ahead, advancements in SBRT technology continue to redefine how prostate cancer is managed. Techniques like the use of fiducial markers and Barrigel spacers have refined its precision. This allows higher doses of radiation to be delivered safely. These innovations reduce treatment-related side effects and improve patient comfort.
Meanwhile, surgical techniques are also evolving. However, they remain inherently invasive, and the associated risks of incontinence and sexual dysfunction are difficult to fully mitigate.
Choosing the Right Approach
Ultimately, the choice between SBRT and prostatectomy is highly individual. It can depend on factors such as age, cancer stage, general health, and personal preferences.
Surgery may remain the best option for younger patients with high-risk disease who desire immediate removal of the cancer. However, for men seeking effective, low-risk, and convenient treatment, SBRT is proving to be a game-changer. It offers an elegant solution that balances cutting-edge technology with a focus on preserving quality of life, making it a compelling option in the modern era of prostate cancer care.
Learn more about Dr Malwinder Singh (The Bald Oncologist)
Website | LinkedIn | Facebook | Instagram | YouTube | TikTok | Spotify

