 By Dennis Thompson
By Dennis Thompson
HealthDay Reporter
WEDNESDAY, Oct. 28, 2020
Average folks should start being screened at age 45 to prevent colon cancer, five years earlier than is now recommended, the nation’s top preventive medicine panel says.
The U.S. Preventive Services Task Force currently recommends that people aged 50 to 75 be regularly screened for colon cancer, one of a handful of cancers that can be prevented outright.
But new data suggests that screening earlier could save even more lives, said task force member Dr. Michael Barry, director of the Informed Medical Decisions Program in the Health Decision Sciences Center at Massachusetts General Hospital in Boston.
“We have epidemiologic data that the risks of colorectal cancer are increasing before age 50, particularly in that 45- to 49-year-old age group,” Barry said.
Computer models suggest that about 25 colon cancer deaths are prevented for every 1,000 Americans between 50 and 75 who are screened, Barry said.
The earlier start is expected to prevent at least one more death per every 1,000 screened, Barry said.
Under the Affordable Care Act, health insurance companies are required to cover the full cost of any screening test recommended by the U.S. Preventive Services Task Force (USPSTF). The task force is an independent, volunteer panel of national experts in prevention and evidence-based medicine.
This guideline covers people at average risk for colon cancer, Barry said. People with factors that put them at higher risk — for example, a strong family history of colon cancer — might need to start screening even earlier, and should discuss it with their doctor.
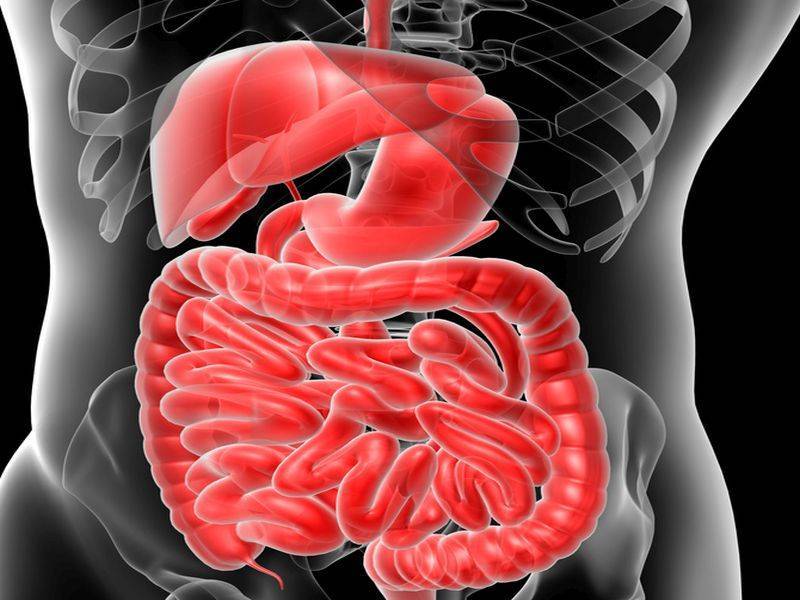
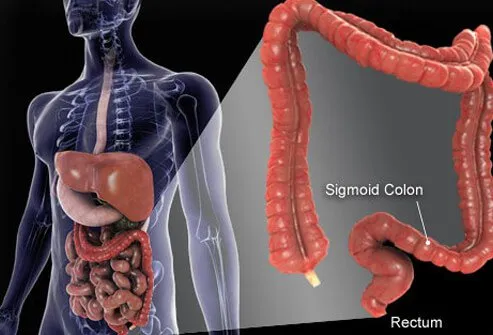
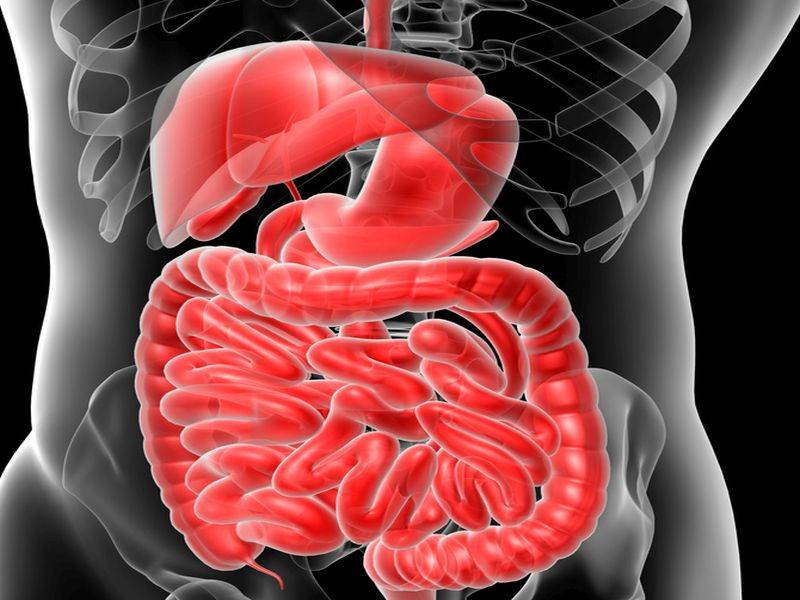
Colon cancer almost always develops from precancerous polyps that form in the colon or rectum. These screening tests detect the presence of these polyps, so they can be removed before they turn into cancer.
Colonoscopy is the most widely known colon cancer screening method, but it’s not the only one, Barry said.
“There are a whole group of tests that can reduce the risk that someone will die of colorectal cancer,” he said.
For example, people can have their stool tested for the presence of tiny amounts of blood, which can indicate the presence of either cancer or polyps.
“That strategy, according to our modeling, can be about as good as colonoscopy in terms of reducing risk,” Barry said.
The frequency a person undergoes screening would depend on the type of test they choose, Barry said. A person with a clean colonoscopy wouldn’t have to be rechecked for a decade, while stool blood tests are often done every one to three years.
When the USPSTF last updated its colon cancer guidelines in 2016, it kept the age at which screening begins at 50 because they were concerned about the strength of the data supporting an earlier start, explained Robert Smith, senior vice president of cancer screening for the American Cancer Society.
The American Cancer Society updated its guidelines in 2018 to recommend that colon cancer screening start at age 45, he added.
“By 2018, we had new data that showed convincingly an increase in incidence in adults under the age of 50,” Smith said. “The data has shown this is a birth cohort effect, and the incidence could be expected to continue to rise.”
The USPSTF updates individual screening recommendations every four years, and “we anticipated when the task group updated their guidelines again in 2020 that they would likely reach the same decision,” Smith said. “The good news now is that they’ve reached the same decision we reached two years ago.”
“Now the public and physicians will have a set of recommendations that are for all practical purposes the same when it comes to when you should begin colorectal cancer screening,” Smith said.
The bad news is that even now people who should get screened are not, Barry and Smith said.
“People do not routinely start screening at the age of 50,” Smith said. “Usually the average age is in the mid-50s. That means during this period of rising incidence we are missing an opportunity to prevent colorectal cancer and detect it early.”
SLIDESHOW
Colon Cancer: Symptoms, Signs, Screening, Stages
See Slideshow
“It looks like about 25% of eligible Americans have not been screened for colorectal cancer,” Barry said. “That will lead to some colorectal cancer deaths that could be prevented, and that’s always a tragedy.”
The USPSTF is taking public comment on this draft recommendation from Oct. 27 through Nov. 23. The task force will consider all comments it receives, and release a final recommendation shortly afterward.
![]()
Copyright © 2020 HealthDay. All rights reserved.
From 
Cancer Resources
Featured Centers
Health Solutions From Our Sponsors
References
SOURCES: Michael Barry, M.D., director, Informed Medical Decisions Program, Health Decision Sciences Center, Massachusetts General Hospital, Boston; Robert Smith, Ph.D., senior vice president, cancer screening, American Cancer Society, Atlanta