Perhaps you’re reading this article because you’re a female powerlifter who has experienced some sort of leaking while lifting. You could also be a coach reading this article to help address this issue for your female athletes. This article is targeted at the lay powerlifter, so medical jargon and expressions will be toned down. Even so, there are still some terms that I hope everyone will have a chance to learn to increase their knowledge in this area.
It is always helpful to have a disclaimer before proceeding. I am a student physiotherapist, not yet trained as a women’s physiotherapist. Most of my understanding about the pelvic floor comes from research and inference from available literature. Feel free to contact us at enso.powerlifting@gmail.com if you have further questions.
Read more about the anatomy of the pelvic floor in our part 1!
What happens when the pelvic floor can’t function properly?
When the pelvic floor malfunctions i.e. weakened or damaged, it leads to an array of conditions termed as pelvic floor dysfunctions/disorders (PFDs).
Can UI be cured?
This will depend on the diagnosis. There are many types of leaking that a person can experience based on the activities they do and the symptoms they have.
Generally, urinary incontinence can be treated with conservative treatment methods i.e. requiring no surgery or hospital stay. Conservative treatments include: bladder training (relearning voiding habits), diet management (caffeine and water intake), exercise regimen (proper rest and exercise intensities) and pelvic floor muscle training (contracting the pelvic floor) for example. More details on these treatment methods will be discussed in the next few parts of the article.
Will urinary incontinence (UI) lead to long-term health concerns?
Data is currently insufficient to determine whether strenuous activities such as powerlifting or resistance training while young predisposes the individual to pelvic floor disorders later in life. Among studies that are available, it is shown that elite athletes—including Olympians—do not experience increased SUI even 15-20 years after their prime. However, they may experience UI earlier in life.
My stance is that it is hard to determine whether a person will experience worse symptoms in the future. Many studies have proven a strong association between pelvic floor symptoms with increased age. It is inevitable that we will experience such symptoms as we age, and some of us may suffer from more severe symptoms. For instance, approximately 50% of elderly women suffer from one or more PFD symptoms.
How common is Stress Urinary Incontinence (SUI)? Is it more common among middle aged women? Can it affect younger women?
Common pelvic floor dysfunctions including urinary incontinence can affect women at all stages of life, from as young as 14 years old to >90 years old. In adolescence, prevalence is low at approximately 10% while for older women >50 years can be as high as 50% (which is half of all women).
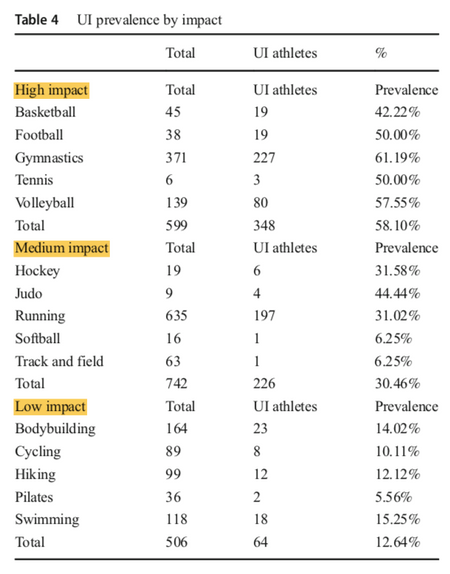
Among female athletes, occurrence rates have proven to be high amongst female athletes in high impact sports like gymnastics, volleyball, soccer and trampolinists. In a recent systematic review, categorization of subjects according to sports impact revealed a positive correlation with urinary incontinence. Generally, high impact sports showed a higher prevalence than low impact sports.
What are the risk factors commonly associated with Stress Urinary Incontinence (SUI)?
Modifiable risk factors are variables that can be modified to manage symptoms of SUI. These include lack of exercise and its contrast, strenuous sporting activities. High physical stress is placed on the pelvic floor when the individual is overweight/obese or suffers from chronic cough. High emotional stresses and anxiety problems contribute to the issue as well. Moreover, soreness and injury in the hip and lower back muscles may affect the function of the pelvic floor too, given that muscle activations during movement don’t happen in isolation.
On the other hand, there are also several unmodifiable factors: increasing age, having one or more children (termed as parity) and existing comorbidities like hypertension and diabetes.
Do sports and exercise help with Stress Urinary Incontinence (SUI)?
The pelvic floor is the only female body part that we are not sure if exercise helps. One idea is that exercise overloads and weakens the pelvic floor, resulting in symptoms of dysfunctions. Another idea is that exercise helps to strengthen the pelvic floor and prevent pelvic floor dysfunctions. Isn’t it weird? Both lack of exercise and strenuous physical activity are risk factors to SUI. Generally, women who exercise have stronger pelvic floors than women who don’t and moderate physical activities like walking, zumba and jogging help to prevent UI. With a stronger pelvic floor it is believed that it will be more capable at keeping the pelvic floor exits closed.
What next?
If you have missed out the first part of the article discussing the anatomy of the pelvic floor, do check it out here! Stay tuned to more information about urinary incontinence in powerlifters in part 3 of this series.
This article and commentary first appeared on ENSO Powerlifting, on May 18, 2020.
