Gout is a form of painful inflammatory arthritis caused by uric acid crystal deposition in the body. Lifestyle changes could help a person with gout live better. Read on to know more!
Epidemiology
Gout is the most common form of arthritis in adults globally, which risk increases with age. It tends to affect men and post-menopausal women more. People of all ethnicities can develop the condition, and an estimated 4%, 2.5% and over 6% of the American, European, and Oceanic Pacific populations are affected by the disease respectively. There has also been growing prevalence of the ailment in the Asian population.
Pathophysiology
When the body produces too much uric acid (also known as urate), or is unable to get rid of it, it results in excessive amounts of uric acid within the blood known as hyperuricemia.
Long-standing hyperuricemia can lead to the accumulation and crystallisation of urate in bones, joints, and tissues. These crystals can in turn trigger the body’s immune system, resulting in an acute ‘gout flare’.
Gout flares are sudden bouts of attacks characterised by severe pain, redness, warmth, and swelling. At times, the pain is so intense and debilitating that it restricts normal daily activities from being carried out. An attack may last between hours to days, and can recur if left untreated, leading to long-standing joint damage.
Single or multiple joints may be affected. But, typically during the initial phase of the disease, only one joint, usually the big toe of the feet, is impacted. Other joints that are commonly affected include the: ankles, elbows, fingers, knees, mid-foot, and wrists.
Over time, if too many crystals collect under the skin, hard and painful lumps called ‘tophi’ develop. This is also known as chronic tophaceous gout.
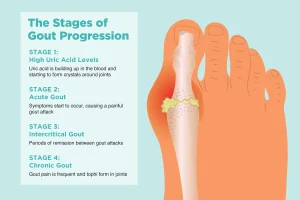
Image credit: https://creakyjoints.org//wp-content/uploads/0919_Stages_Gout.jpg
Diagnosis
It is important to get an accurate diagnosis by ruling out alternative causes, as other forms of joint disease or injuries can potentially take on the presentation of gout as well.
The preferred approach to determining if a person has gout is through analysing the synovial fluid of their joint under a microscope for the presence of urate crystals.
If synovial fluid examination is not possible, doctors can also make use of other clinical, laboratory, and radiologic findings to detect if someone has gout.
| Type of Investigation | Example |
| Clinical | Signs and symptoms Physical examination |
| Laboratory | Blood uric acid levels |
| Radiological | Computed tomography (CT) scan Ultrasound |
Management of gout
Lifestyle Modifications
A person’s quality of life can be affected significantly due to the pain, and potential joint damage as well as deformity that gout can cause. Apart from medical therapy, lifestyle changes can also help to manage the illness better.
Diet
Purine is a compound found in food, in particular those rich in protein, which is broken down into uric acid within the body, hence raising uric acid levels in the blood. As previously mentioned, high uric acid levels in the blood can lead to hyperuricemia which could trigger gout.
Animal-based meats and seafood (e.g., liver and kidney, red meats – pork, beef, and lamb, sardines, shellfish), and certain plant-sourced foods (e.g., legumes, mushrooms, nuts, soy) are rich in purines.
Sweetened beverages, especially those that contain high amounts of fructose, can increase the body’s uric acid production and therefore might contribute to hyperuricemia.
Alcohol consumption have also been associated with higher risk for flares, and its intake should therefore be moderated (e.g., Limit of 2 servings for men and 1 serving for women). However, in the event of an attack, or in poorly controlled disease, alcohol should be avoided.
There is also evidence showing that intake of low-fat dairy products could reduce uric acid levels, leading to a lower incidence of gout, and might potentially reduce gout flares as well.
At present, there are no well-established guidelines to recommend a diet specific for patients. But improving dietary habits could help to reduce gout flares, thereby enhancing a person’s quality of life. In addition, generally, having well-balanced meals will benefit overall health.
Weight loss
If a person is overweight, watching what they eat can also help them achieve a healthier weight. Studies have shown that weight reduction towards ideal body weight, especially for those who are overweight/obese, can reduce serum urate concentrations, frequency of gout, and its associated flares.
Diet modifications alone may also not be sufficient for urate control but coupled with weight loss in those who are overweight, could bring about more significant improvement in urate control.
Pharmacological Treatment
During acute events, anti-inflammatory agents are used to resolve each episode quickly and safely. Treatment is most effective when started early in the course of the flare and is temporary, limited to the period of the attack.
Some of the commonly used drugs are as follows:
- Colchicine
- Non-steroidal anti-inflammatory drugs (NSAIDs) (e.g. diclofenac, ibuprofen, naproxen, indomethacin, etoricoxib, celecoxib)
- Systemic corticosteroids (e.g. prednisolone, methylprednisolone)
Maintaining low uric acid levels in the blood is essential to prevent further formation of urate crystals and allow dissolution of existing ones.
In addition, for individuals who have more advanced stage of the disease e.g., frequent painful flares, joint damage, tophi, long-term urate lowering therapy is recommended.
Some of the commonly used drugs are as follows:
- Agents that reduce production of uric acid: Xanthine-oxidase inhibitors – blocks the substance (xanthine-oxidase) that is involved in the production of uric acid (e.g. allopurinol, febuxostat)
- Agents that promote elimination of uric acid: Uricosuric agents – increase urinary excretion of uric acid (e.g. probenecid, benzbromarone)
- Agents that break down uric acid: Uricase – converts uric acid to another form that can be removed by the body more easily (e.g. pegloticase, rasburicase)
Management of gout needs to be tailored to the individual. Some may involve the use of a combination of drugs in addition to lifestyle changes, so make sure to discuss your condition thoroughly with your healthcare provider. Ensure your clinician is informed of other concurrent illnesses and medications, allergies, and concerns that you might have which could affect your therapeutic plan.
