A new telemedicine initiative, OPTIMUM (Optimising care of Patients via Telemedicine In Monitoring and Augmenting their control of Diabetes Mellitus), is showing promise as a power tool in diabetes management, providing patients with tools for better self-care, enhanced monitoring, and ultimately improved health outcomes.
Read also: 6 in 10 Singaporeans with Diabetes Have Poor Glucose Control, Survey Finds
OPTIMUM Study: Patient-Provider Collaboration in Diabetes Management
Developed by SingHealth Polyclinics in collaboration with the MOH Office for Healthcare Transformation (MOHT), OPTIMUM leverages technology to give patients a proactive role in managing their health.
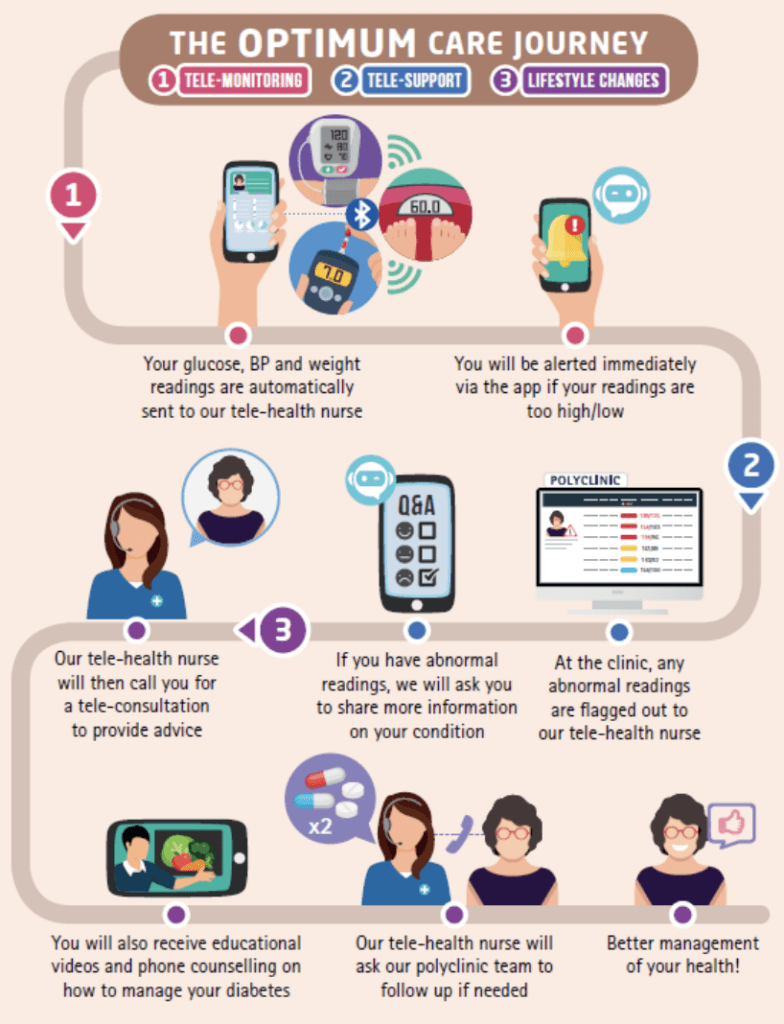
Over a six-month clinical study conducted at SHP-Sengkang, 160 patients with T2DM used the OPTIMUM telemonitoring system, which includes a suite of Bluetooth-enabled devices — a weighing scale, a glucometer, and an electronic blood pressure monitor. All these devices sync with an easy-to-use OPTIMUM app on their phones.
The patients received a structured programme through the OPTIMUM app that consists of:
- Weekly push notifications to encourage self-monitoring
- Educational videos covering self-management topics on diabetes mellitus such as healthy eating, mindset strategies, physical activity demonstrations and more
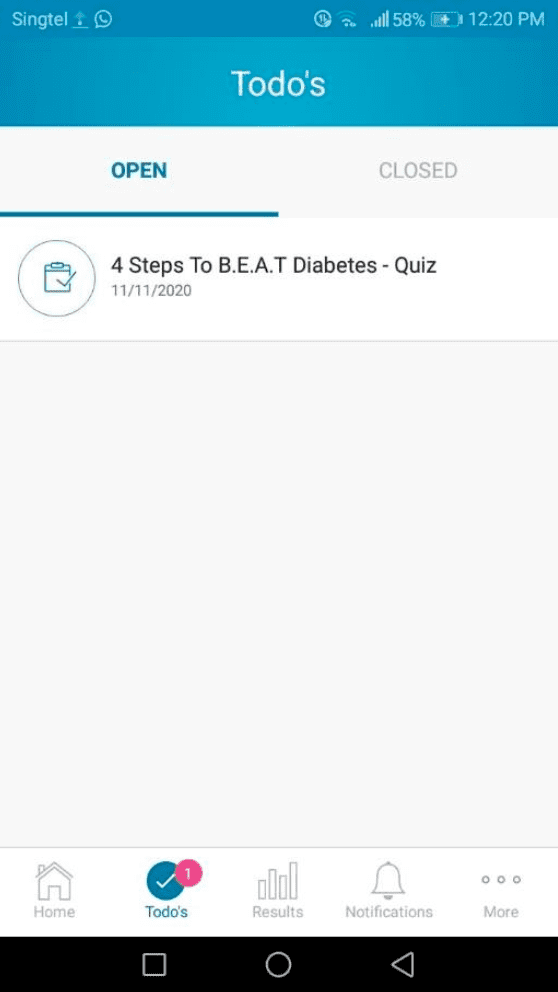
- Quizzes after video materials to assess understanding
“We actually co-design (the application) with patients…Even before we roll out this, patients have an input into what they want the platform to do for them.” This patient-centric and culturally-adapted design ensures that the platform is most relevant and user-friendly for patients.
Self-monitoring and Remote Monitoring
This study, one of the first of its kind in Singapore, assessed not only physical metrics like blood pressure and cholesterol but also quality of life and self-management skills.
As part of the self-monitoring, patients tracked their body weight, blood pressure, heart rate, and capillary glucose levels with their Bluetooth devices over the six-month trial. These data are fed to the clinician dashboard within the OPTIMUM system.
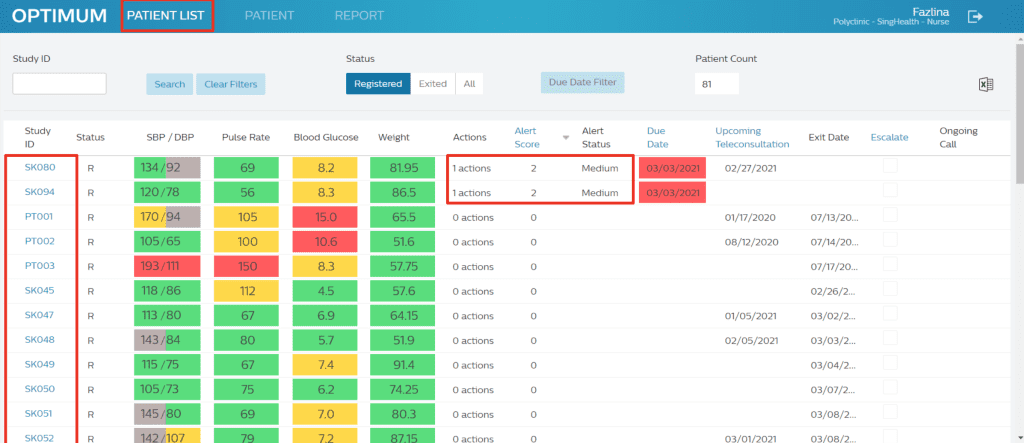
Should readings fall outside the normal range, patients will receive prompt feedback via the app to confirm their readings, report symptoms and even check on their medication use. This real-time feedback loop helps patients take corrective actions and provides them with peace of mind.
Healthcare providers are also able to monitor patients remotely via the dashboard. As part of the study, nurses closely monitor the patients and implemented actions based on protocol, involving teleconsultations and even physician review.
Proactive Health Monitoring to Manage Diabetes

“The OPTIMUM app is valuable for me, as I often struggle to keep track of my blood sugar
levels. By utilising this app, I’ve been able to take a more proactive approach to managing
and controlling my health,” shared Ms Vasudeva Sujatha Menon, 62, a patient of SHP-
Sengkang who participated in the study.
For patients like Ms Vasudeva, regular self-monitoring has translated into tangible health improvements. Results from the trial show that OPTIMUM patients achieved better control over their health in more ways than one.
From their HbA1c levels, blood pressure, to total cholesterol levels, improvements are greater compared to those receiving standard care.
The intervention group saw :
- Substantial reduction of 0.34% in HbA1c levels compared to the control group
- 3 mmHG lower in average systolic blood pressure
- 0.17 mmol/L point difference in total cholesterol
- Five times more likely to adhere to prescribed medication
- Significantly higher score on the Self-Care Inventory-Revised (SCIR), indicating enhanced self-management and care practices.
These results suggest that the OPTIMUM system effectively supports patients with Type 2 Diabetes — not only improving blood glucose, but also other health indicators and even self-care.
Patient Education and Empowerment in Diabetes Management
A standout feature of OPTIMUM is its educational component. Patients receive weekly notifications with locally produced videos on topics such as diet, exercise, and medication management. Each video is followed by a quiz to reinforce learning.
One of the videos integrated into the OPTIMUM app
This approach aims to improve diabetic literacy, a crucial element in effective long-term disease management.
“This advancement in diabetes care aims to empower patients and enhance their management of
the condition, ultimately leading to better health outcomes for those living with T2DM in
Singapore,” says Dr Lee Cia Sin, Family Physician (Consultant), SHP-Sengkang. Dr Lee was one of the key research investigators on-site for this research study.
This was echoed by the patients, who felt the understanding of their condition helped to shape the way they manage their health.

“I (didn’t) have much understanding of these things like exercises, food intake,” said Mr Faridon Abd Aziz, 61, also a patient of SHP-Sengkang who participated in the study.
He shared candidly — “They sort of force me to watch this video and then have a question to see my understanding of the video, and (I) may understand better.”
“Exercising is important, food intake is important, regular medication is important.”
Some patients may be concerned about using new technology and equipment, especially those who are less tech-savvy. Both Mr Faridon and Ms Vasudeva shared that this was unfounded.
“We were all 60s babies, and we don’t know anything about apps and all those things,” Ms Vasudeva said. “(But) after learning from them, I was able to use it.”
What’s Next For OPTIMUM?
Following the study’s promising results, MOHT has already expanded upon the success of OPTIMUM by incorporating its methods into the Primary Tech-Enhanced Care – Diabetes Mellitus (PTEC-DM) programme, which launched across four polyclinics in 2023.
“We gained from the trial the lessons, and then we transplant it into the PTEC-DM programme.” Prof Gerald Koh, Clinical Director and Head (Future Primary Care), MOHT.
Early feedback has been positive, paving the way for more polyclinics to adopt similar telemedicine-based solutions.
The future of diabetes care in Singapore may very well include a more widespread adoption of tools like OPTIMUM, which not only improve clinical outcomes but also lower long-term healthcare costs.
“While there were initial costs for equipment and professional coaching, the long-term savings
in healthcare expenses are promising.” remarks Clinical Associate Professor (Dr) Tan Ngiap Chuan, Director of Research and Primary Care Research Institute (PCRI), SHP and Vice-chair, Research, SingHealth-Duke NUS Family Medicine Academic Clinical Programme (FM ACP).
The benefits and improved health outcomes, in fact, continued even after the telemonitoring phase ended, In the following 18 months, there are still sustained improvements in health and medication adherence.
“The real value of OPTIMUM lies in the behavioural changes it promotes, encouraging patients to take ownership of their health.”
As diabetes continues to pose a major health concern, Singapore’s healthcare system is finding new ways to empower patients through technology. OPTIMUM is a step forward in leveraging telemedicine to manage chronic diseases like diabetes, and paves the way for a future of patient-centered, digitally enabled care.
When asked if he would be open to use such a telemedicine model forever, Mr Faridon smiled. “I don’t mind.”

