Proteins like IL-31, nerve hypersensitivity and barrier weakness shape the intense itch of atopic dermatitis. The interplay between skin, nerves and immunity explains why the itch feels so persistent.
Itching, also medically known as pruritus, may seem like a trivial annoyance. However, for millions of people living with chronic skin conditions such as atopic dermatitis (AD), the itch is far more than that.
Itch in AD is an intense biological reaction powered by misfiring nerves, overactive immune messengers, and a weakened skin barrier. It is a symptom that reveals a deeper breakdown in how the skin communicates with the body.
Let’s reveal the strange science of scratching — how it starts, how it spirals, and why that itch is never “just” an itch.
What is Atopic Dermatitis?

Atopic dermatitis (AD) is a long-term skin condition that causes dry, inflamed and intensely itchy skin. It is the most common type of eczema (a group of skin conditions that result from inflammation).
It often appears as reddish or brownish patches, scaly or thickened skin, and small bumps that crust over or even ooze fluid.
Although symptoms vary between individuals, the rash can appear anywhere on the body, particularly in skin folds. It may also affect both children and adults.
Common symptoms of AD include:
- Skin rash
- Dry, cracked skin
- Itchy skin (ranging from mild to severe)
- Crusting
- Swelling
- Skin discolouration (e.g. red or brown patches on the affected area)
Understanding the Biology of Itch
Itch is the hallmark symptom of atopic dermatitis (AD). Nearly everyone living with AD reports itching as a major concern.
Itch signals travel along their own neural pathways. There are nerve fibres that respond specifically to itch-related molecules.
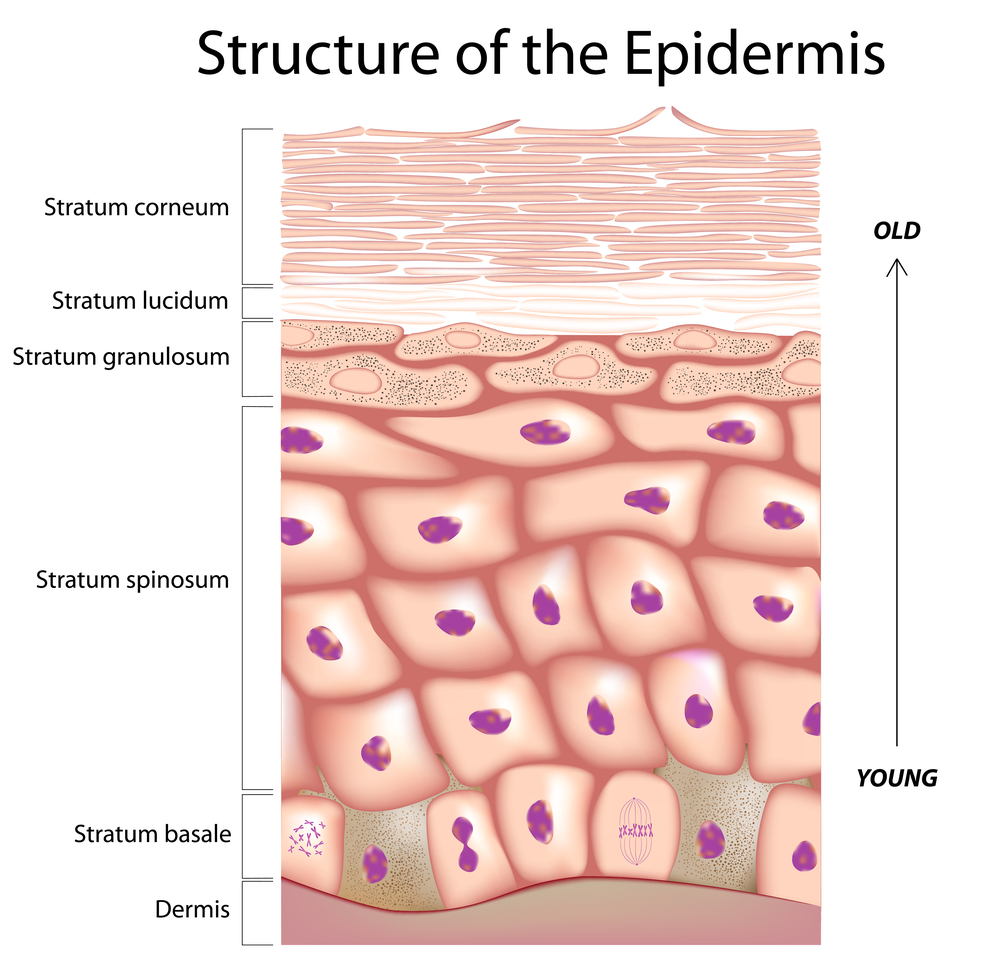
In healthy skin, the outermost cells form a strong barrier called stratum corneum. It keeps foreign materials (e.g. bacteria, allergens) out of the skin. Beneath the epidermis lie the nerve endings in the dermis layer.
In AD, the skin barrier is compromised. Irritants and pathogens can penetrate the skin, triggering inflammation. This prompts skin cells (keratinocytes) and immune cells to release chemical messengers that bind to nerve receptors, transmitting signals to the brain and producing the itch sensation.
Key players involved in itch include:
- Kallikreins (KLK): Enzymes that normally help the skin to shed dead cells to prevent thickening. In AD, certain kallikreins (e.g. KLK7, KLK8, KLK10 and KLK11) become overactive, causing too much skin shedding and weakening the skin barrier.
- Interleukin-4 (IL-4) and Interleukin-13 (IL-13): Cytokines that promote inflammation and increase nerve sensitivity to itch sensations.
- Interleukin-31 (IL-31): An “itchy” cytokine (messenger proteins) that directly activates itch receptors on sensory neurons. IL-31 is released by several types of immune cells. The combination of a weakened barrier and elevated IL-31 creates a perfect storm in which itch nerves are repeatedly stimulated.
IL-31: The “Itchy” Cytokine
Unlike other immune chemicals that cause swelling or redness, IL-31’s main target is the nerves that send itch signals to the brain. People with atopic dermatitis tend to express higher levels of IL-31 because their immune system is more active.
Here is why IL-31 plays such a big role in AD:
1. It switches on the itch nerves directly
IL-31 attaches to special receptors on the skin’s sensory nerves, almost like turning on a light switch. Once activated, these nerves send a strong itch signal straight to the brain.
2. It makes the nerves extra sensitive
When IL-31 levels are high, the nerves become even more sensitised. This means even small stimuli – a bit of sweat, heat, tight clothes, stress, or minor friction – can trigger intense itch. What feels like nothing to others can feel unbearable for someone with AD.
3. It encourages more scratching.
Scratching then damages the skin barrier, leading to more irritation and inflammation, which causes the body to release even more IL-31. This creates a loop where itch leads to scratching, and scratching leads to more IL-31, which triggers even more itch.
Itching and Scratching

We’re all familiar with the temporary pleasure of scratching an itch. When itching occurs, the instinct to scratch provides short-lived relief.
Two types of nerve activity are involved when a person experiences itch and scratch behaviour:
- GABA (gamma-aminobutyric acid) nerves that process an uncomfortable sensation of itch.
- DA (dopaminergic) nerves that mediate the pleasure response to scratching.
The brain’s reward system is activated, giving an intense sense of satisfaction but this relief comes at a cost. Scratching damages the skin further, worsens inflammation, and triggers more itching.
Because of this, many patients say the itch feels:
- “relentless”,
- “unpredictable”, or
- “like it comes from underneath the skin”
IL-31 is one of the main reasons atopic dermatitis itch is so difficult to control.
 Do you have eczema or know someone who does? Medical Channel Asia is conducting a short 5-min survey to understand how eczema and itch affect daily life in Singapore. Leave your contact details and stand a chance to receive a wellness pack as a token of our appreciation!
Do you have eczema or know someone who does? Medical Channel Asia is conducting a short 5-min survey to understand how eczema and itch affect daily life in Singapore. Leave your contact details and stand a chance to receive a wellness pack as a token of our appreciation!
How Doctors Measure Itch Objectively?
Measuring itch is uniquely challenging because it is a subjective sensation. Doctors use validated assessment tools to evaluate the itch.
1. Unidimensional Itch Intensity Scales
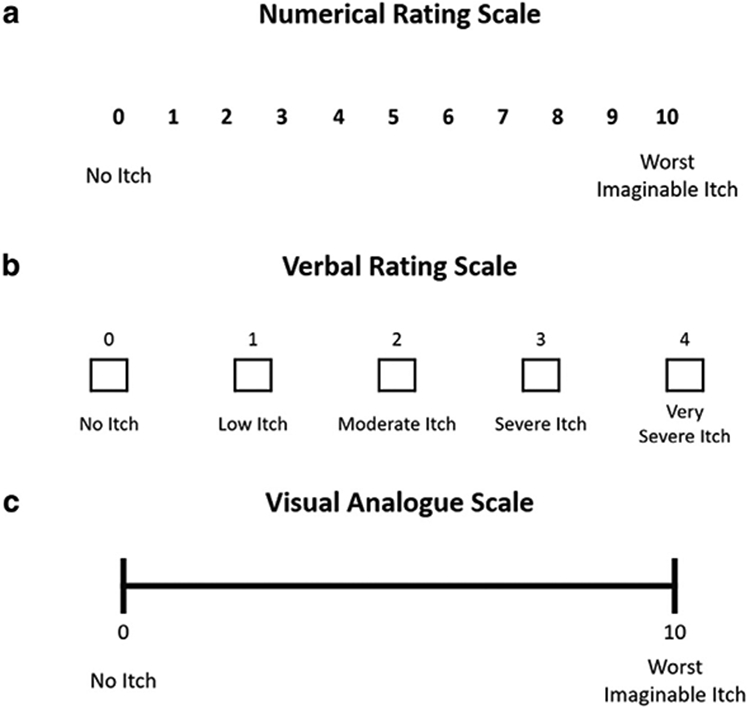
Unidimensional scales focus solely on itch intensity, relying on self-reporting by patients.
- Numerical Rating Scale (NRS): Itch intensity is rated between 0 (no itch) to 10 (worst imaginable itch) over a given period.
- Verbal Rating Scale (VRS): Itch is rated using five categories, from 0 (no itch) to 4 (very severe itch).
- Visual Analogue Scale (VAS): A continuous line marked from 0 (no itch) to 10 (worst imaginable itch). Patients can indicate their perceived itch intensity on the line.
They are simple but effective in tracking fluctuations over days or weeks.
2. Peak Pruritus Numerical Rating Scale (PP-NRS)
As one of the most used scales, PP-NRS measures the worst itch experienced over the past 24 hours. Patients are asked to rate their itch on a scale from 0 to 10:
- 0 = No itch
- 10 = Worst imaginable itch
A change of at least 4 points on the PP-NRS is considered clinically meaningful improvement.
The scale is simple, reliable, and suitable for self-assessment.
3. 5-D Itch Scale
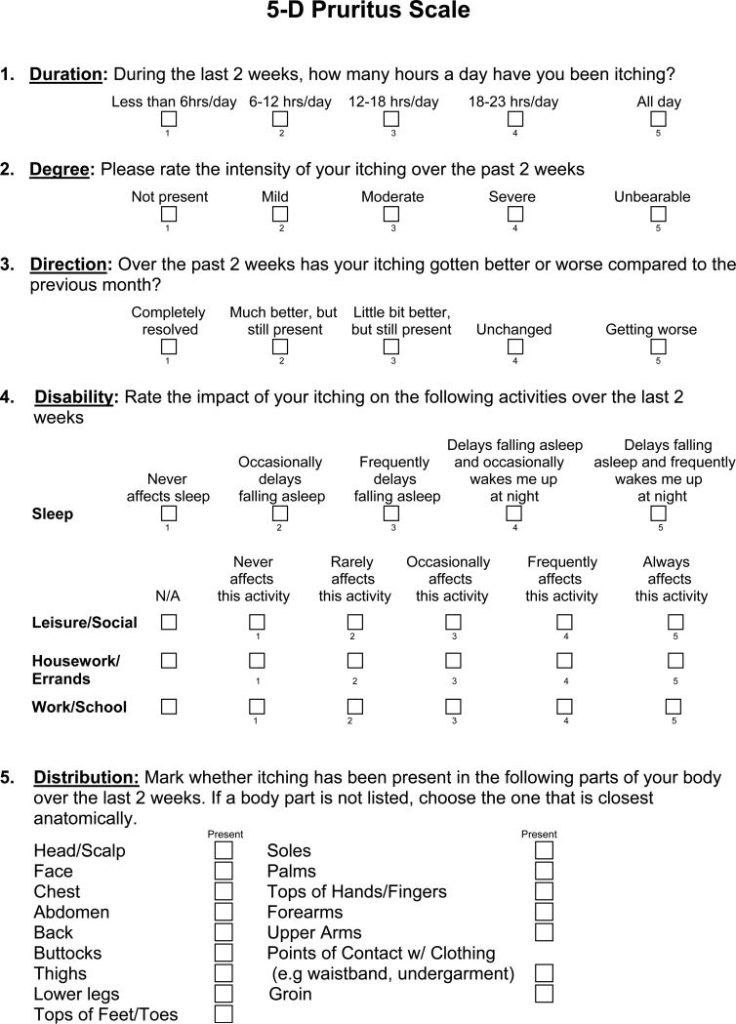
5-D itch scale evaluates five dimensions. It paints a fuller picture of how itch affects daily function, sleep, and physical movement. The five dimensions include:
- Duration
- Degree
- Direction (improving or worsening)
- Disability
- Distribution
Higher scores indicate more severe itch. This tool is validated for use in atopic dermatitis and other chronic itch conditions.
Why Itch Deserves Far More Attention
Pain often receives more medical urgency because it signals immediate harm. But chronic itch can be equally disruptive. It affects mood, sleep quality, interpersonal relationships, work performance, and in children, behaviour and learning.
Importantly, itch also serves as a sign of deeper dysfunction.
When itch is incessant, it indicates an imbalance between:
- the skin barrier
- the body’s immune system
- the neural pathways that interpret sensory signals
In short: itch matters. It reveals the connection between the skin, nerves, and the immune system. There is good news too – the science behind itch has contributed to treatment advancements as well.
Treatment options now target different points in the itch pathway, from repairing the skin barrier to calming inflammation and, in more recent years, addressing the chemical messengers that trigger nerve activation. Moisturisers, anti-inflammatory medicines, and targeted biologics are all part of the growing toolkit doctors use to break the itch cycle.
While effective treatment can look different for everyone, understanding the drivers of itch allows dermatologists to personalise treatment based on severity and triggers. With the right plan, many people experience meaningful relief and fewer flare-ups, proving that chronic itch does not have to be a lifelong struggle.
Visit our Dermatology Chapter – Atopic Dermatitis for more information and resources on living with eczema and chronic itch.
References
- Atopic Dermatitis. Cleveland Clinic. Updated: 3 April 2025. https://my.clevelandclinic.org/health/diseases/24299-atopic-dermatitis
- The Never-Ending Itch: Living with Atopic Dermatitis. Medical Channel Asia. Updated: 20 October 2025. https://medicalchannelasia.com/the-never-ending-itch-living-with-atopic-dermatitis/
- The Complex Science Behind Itch in Atopic Dermatitis. National Eczema Association. Updated: 3 January 2023. https://nationaleczema.org/blog/science-of-itch/
- Erickson S, Kim BS. Research Techniques Made Simple: ltch Measurement in Clinical Trials. J Invest Dermatol. 2019 Feb; 139 (2): 264 – 269. https://pmc.ncbi.nlm.nih.gov/articles/PMC8922716/
- Yosipovitch, G., et al (2019). Peak Pruritus Numerical Rating Scale: psychometric validation and responder definition for assessing itch in moderate-to-severe atopic dermatitis. The British journal of dermatology, 181(4), 761–769. https://pmc.ncbi.nlm.nih.gov/articles/PMC6850643/
- Elman, S., Hynan, L. S., Gabriel, V., & Mayo, M. J. (2010). The 5-D itch scale: a new measure of pruritus. The British journal of dermatology, 162(3), 587–593. https://pmc.ncbi.nlm.nih.gov/articles/PMC2875190/
- Kabashima, K., & Irie, H. (2021). Interleukin-31 as a Clinical Target for Pruritus Treatment. Frontiers in medicine, 8, 638325. https://doi.org/10.3389/fmed.2021.638325
- Lugović-Mihić, L., Meštrović-Štefekov, J., Potočnjak, I., Cindrić, T., Ilić, I., Lovrić, I., Skalicki, L., Bešlić, I., & Pondeljak, N. (2023). Atopic Dermatitis: Disease Features, Therapeutic Options, and a Multidisciplinary Approach. Life (Basel, Switzerland), 13(6), 1419. https://doi.org/10.3390/life13061419

