Mpox, formerly known as monkeypox, is a rare disease that is caused by infection with the monkeypox virus, which is closely related to the infamous smallpox virus.
It was first discovered in 1958 with two outbreaks in colonies of monkeys. The first human case was confirmed in 1970 in Congo, Africa. Since the 1970s, many cases have been reported elsewhere in Africa, and occasionally in the US or Middle East through international travel.
The World Health Organization (WHO) declared on 11 May 2023 that the mpox outbreak is no longer a global health emergency, reversing the declared status from July 2022. From January 2022 through April 2023, more than 87,000 confirmed cases of mpox, including 140 deaths, were reported to WHO from 111 countries or territories. Globally, cases have been declining as awareness has increased and a vaccine become widely available. The emergency committee in WHO decided to lift the status as they decided that the challenges posed by mpox were best solved through a long-term approach rather than through emergency measures, considering the huge gaps in knowledge and continued lack of effective treatment.
How does mpox spread?
Mpox virus is transmitted from one person to another by close contact with body injuries, body fluids, respiratory droplets, and contaminated objects. Unlikely its COVID counterpart, it is much less infectious. Usually, the incubation period is from 1 to 2 weeks.
Animal-to-human transmission may occur through direct bite or scratch, direct or indirect contact with body fluids or lesion material. Many animal species can be susceptible to mpox virus, thus eating undercooked animal meat can also result in human infection.
Mpox gets the name because it was first identified in lab monkeys. However, we are not sure about the main reservoir host of mpox, African rodents are suspected to play a key part in transmission.
What are the signs and symptoms?
Signs and symptoms of mpox are very similar to smallpox. Key symptoms to pay attention to:
- Fever and chills
- Headache
- Muscle aches
- Backaches
- Joint pain
- Swollen armpit
- Extreme lethargy
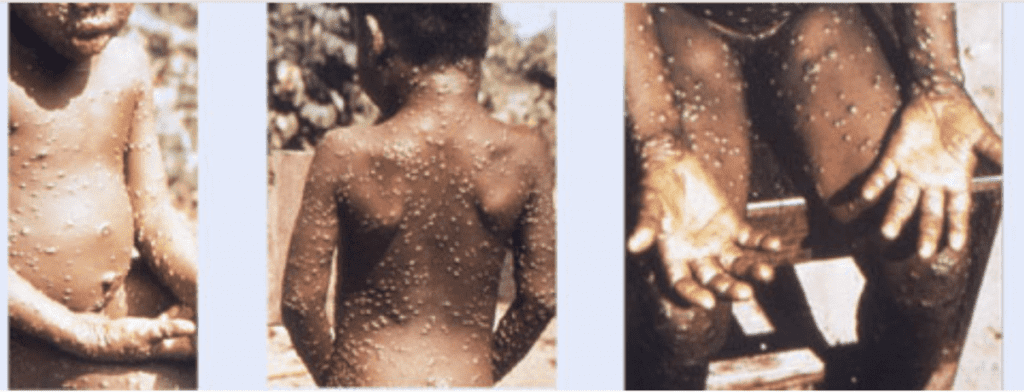
Within 1 to 3 days of presentation, most patients would develop a rash, often beginning on the face and then spreading to other parts of the body.
Lesions progress through the following stages before falling off:
- Macules
- Papules
- Vesicles
- Pustules
- Scabs
The disease usually progresses around 2 to 4 weeks. In African endemic regions, 1 in 10 people infected with mpox will die.
Prevention and treatment
Despite the status being reversed, WHO Director-General Tedros warned that “as with Covid-19, that does not mean that the work is over. Monkeypox continues to pose significant public health challenges that need a robust, proactive and sustainable response”.
There is no proven anti-viral treatment for mpox developed so far. However, a licensed vaccine that protects against mpox and smallpox Bavarian Nordic’s Jynneos – was approved by the FDA in 2019 for adults aged 18 years or older in the US. US CDC recommends vaccination against mpox if:
- You had known or suspected exposure to someone with mpox
- You had a sex partner in the past 2 weeks who was diagnosed with mpox
- You are a gay, bisexual, or a man who has sex with men or a transgender, nonbinary, or gender-diverse person who in the past 6 months has had any of the following:
- A new diagnosis of one or more sexually transmitted diseases (e.g., chlamydia, gonorrhoea, or syphilis)
- More than one sex partner
- You have had any of the following in the past 6 months:
- Sex at a commercial sex venue (like a sex club or bathhouse)
- Sex-related to a large commercial event or in a geographic area (city or county for example) where mpox virus transmission is occurring
- Sex in exchange for money or other items
- You have a sex partner with any of the above risks
- You anticipate experiencing any of the above scenarios
- You have HIV or other causes of immune suppression and have had recent or anticipated future risk of mpox exposure from any of the above scenarios
- You work in settings where you may be exposed to mpox:
- You work with orthopoxviruses in a laboratory
Other than vaccination, lifestyle cautions can also help to avoid infection:
- Avoid contact with animals, especially those that look sick or have been found dead
- Avoid contact with known cases and self-isolate if you are a close contact
- Avoid contact with materials that might have been touched by an animal or person with a known monkeypox infection
- Wash your hands often before and after touching your face, and before eating
- Use personal protective equipment when entering high-risk places like hospitals or animal farms
In hospital settings, symptomatic control including anti-fever and painkiller medications will be given. Patients with severe symptoms could potentially be eligible for an organ support system as well.