Polycystic Ovarian Syndrome (PCOS) is a common hormonal disorder affecting 10% of women of reproductive age. The hormonal disarray in PCOS presents as a syndrome or group of symptoms affecting the ovaries and ovulation, usually coupled with weight gain and metabolic complications, posing far-reaching implications on health beyond reproductive function.
What are the main features of PCOS?
The 3 main features are:
- Increased levels of male hormones (androgens) or hyperandrogenism: Excess male hormones may result in physical signs like excess facial and body hair (hirsutism), acne and male-pattern baldness.
- Irregular menstrual periods
- Hyperandrogenism inhibits ovulation, which is the monthly release of mature eggs from the ovaries.
- Lack of ovulation can cause irregular menstruation e.g. <9 periods a year or > 35 days between periods and abnormally heavy periods
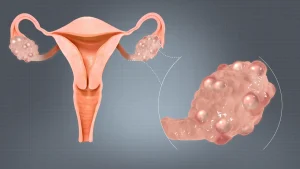
- Cysts in the ovaries
- The many unreleased eggs in the ovaries form cysts, thereby result in the characteristic polycystic appearance of the ovaries.
Diagnosis of PCOS
A diagnosis of PCOS is made if a woman presents with at least 2 out of 3 of the abovementioned features. There is no definitive diagnostic test, but the following may be done:
Blood tests to measure hormone levels
- e.g. high levels of testosterone coupled with physical features of hirsutism or acne are suggestive of PCOS
- Many conditions can mimic PCOS and may be ruled out with relevant labs. For e.g.:
- Thyroid-stimulating hormone (TSH) to rule out a thyroid disorder
- Cortisol to rule out Cushing’s syndrome
Review of medical history
The doctor will solicit information regarding the regularity of your menstrual period and weight changes.
Pelvic examination +/- ultrasound
The doctor manually inspects your reproductive organs for masses or abnormalities. Ultrasound may be done to check the appearance of the ovaries (polycystic, enlarged with multiple cysts) or thickness of the uterus lining (endometrium).
What causes PCOS?
The exact cause is unknown but some factors that may be involved include:
- Genes: Studies show a familial link – you are more likely to have PCOS if your sister or mother has it.
- Insulin resistance
- Up to 70 percent of women with PCOS have insulin resistance, meaning that their cells cannot respond well to insulin.
- Insulin is the hormone produced in the pancreas that enables cells to utilise sugar/take up glucose from blood for energy supply; failure to do so causes blood sugar levels to rise which in turn triggers the pancreas to produce more insulin.
- Excess insulin sparks an increase in androgen production (hyperandrogenism), inhibiting ovulation.
- Inflammation
- PCOS has been linked with higher levels of inflammatory markers.
- One possible source of inflammation could be excess visceral adipose tissue – the fat that accumulates deep in the abdomen and around the organs
- This inflammation causes hyperandrogenism and ovarian dysfunction.
Complications of PCOS
Reproductive
- Infertility
- Lack of regular ovulation makes it difficult to conceive; PCOS is a leading cause of infertility.
- If able to conceive, pregnancy complications include risk of gestational diabetes, pre-eclampsia (high blood pressure during pregnancy) and miscarriage.
- Endometrial cancer
- During ovulation, the uterine lining sheds. Without ovulation, the lining can build up, increasing your risk for endometrial cancer.
Metabolic
Insulin resistance is a key driver in the development and progression of PCOS, especially the metabolic complications.
- Diabetes: Insulin resistance causes blood sugars to increase, predisposing to type 2 diabetes.
- Obesity: Insulin resistance and hyperandrogenism can cause weight gain and obesity; this in turn further aggravates the inflammation, metabolic issues and reproductive abnormalities in PCOS.
- Metabolic syndrome: PCOS sufferers are at higher risk of developing this cluster of conditions including high blood pressure, high blood sugar, and abnormal cholesterol or triglyceride levels that significantly increase the risk of heart diseases and stroke.
Physical
The increased levels of androgens can lead to development of more masculine traits.
- Hirsutism: Excess hair that is darker and coarser on the face, chest, or back
- Acne, due to oilier skin more prone to breakouts
- Male-pattern hair loss (thinning of hair on the head)
Increased levels of insulin can result in
- “Acanthosis Nigricans” – Dark discolouration or patches in body folds like the back of neck or armpits
Psychological
The hormonal changes and impact on physical appearance predispose PCOS sufferers to negative emotions, anxiety and depression.
Others
- Sleep apnea
- This is a condition in which breathing stops involuntarily for brief periods of time during sleep.
- Narrowed airway due to obesity obstructs the flow of air; the risk for sleep apnea is 5 – 10 times higher in women who have both obesity and PCOS than in those without PCOS.
- Sleep apnea in turn also increases risk of heart diseases and stroke.
Treatment
Treatment is focused on addressing symptoms and preventing complications as there is no single cure for PCOS.
Medications
- Oral contraceptive pills may help to correct the hormonal imbalance, regulating ovulation and menstruation, lowering testosterone levels thus treating acne and hirsutism, also lowering risk of endometrial cancer.
- Antibiotics and retinoid creams may be helpful for acne
- Metformin can reduce insulin resistance and blood sugar levels; it can also stimulate ovulation and regulate periods.
Aesthetic procedures
Excessive hair growth can be addressed by shaving, waxing, laser treatment, bleaching, electrolysis, or topical depilatories.
Lifestyle changes
- Weight loss through regular exercise and dietary discretion can reduce insulin resistance and consequent hyperandrogenism, as well as complications of PCOS.
- Adopt a low-calorie diet:
- Avoid processed foods/snacks (sweetened juices, biscuits, frozen pizzas) and opt for fresh foods (e.g. recommended daily servings of fruit)
- Avoid refined sugars (white bread, white rice) and choose complex carbohydrates (wholegrain bread/pasta, brown rice) which are digested more slowly and are less likely to cause spikes in sugar levels
- Reduce carbohydrate intake overall and take more lean meats and healthy fat (fatty fish like salmon high in omega-3)
Conclusion
Most women with PCOS are able to lead a normal life without significant complications if they seek timely treatment, alongside appropriate lifestyle changes.

