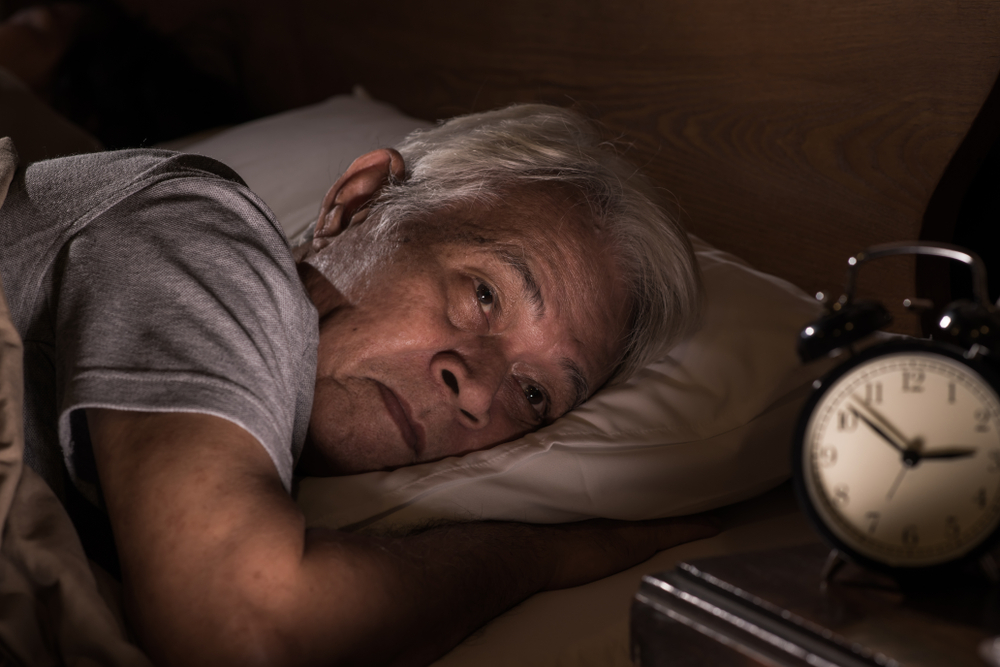
Noticing that your sleep is not what it used to be as you get older?
If you have ever wondered why elderly sleep less, it is not just in your head. Many older adults find that sleep becomes lighter, shorter, or more fragmented with age, even if they are spending the same amount of time in bed.
Ageing brings natural changes to the body that affect when we feel sleepy, how deeply we sleep, and how easily we wake up at night. On top of that, health conditions and lifestyle shifts later in life can further interfere with rest. Understanding why these changes happen can help older adults and their families set realistic expectations and take steps to support better sleep.
Do Older Adults Need Less Sleep?
It is a common misconception that older adults need less sleep. In reality, most adults, including seniors, still need around seven hours of sleep per night.
The issue is not a reduced need for sleep, but rather difficulty achieving consistent, high-quality rest. Changes in the body’s internal clock, medical conditions, medications, and daily routines all contribute to why sleep becomes more challenging with age.
How Does Ageing Affect Sleep?
Biological & Hormonal Changes
One of the main reasons why elderly sleep less lies in changes to the body’s internal clock, also known as the circadian rhythm. This clock is regulated by a small area in the brain called the suprachiasmatic nucleus (SCN), which helps control sleep timing, hormone release, and alertness across a 24-hour cycle.
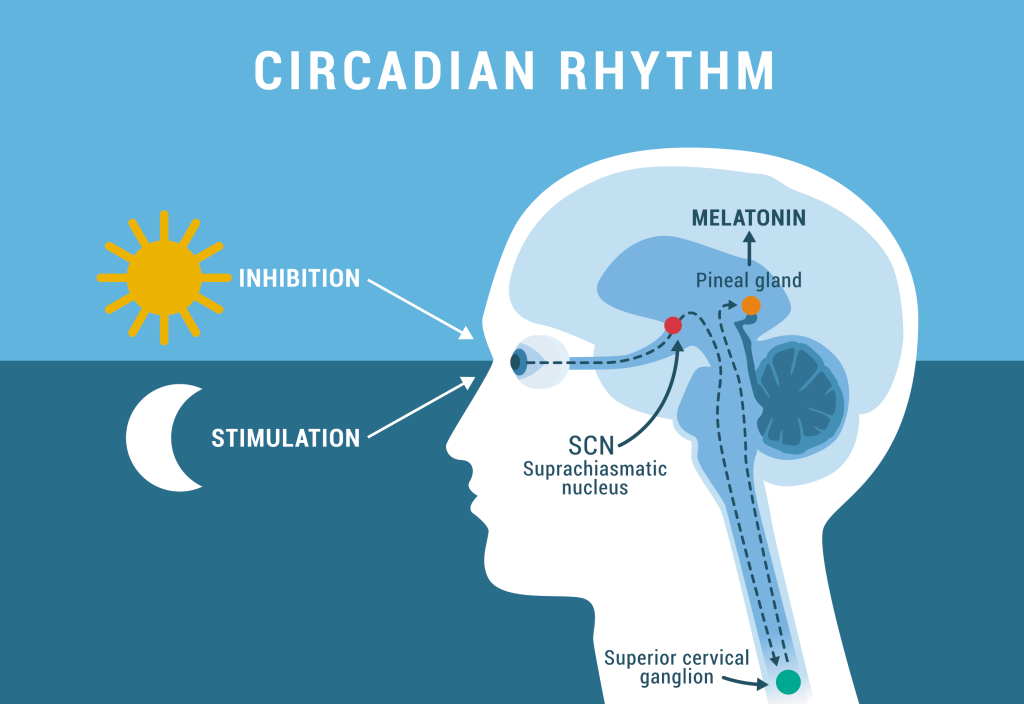
As people age, the SCN becomes less efficient. This can cause a shift in sleep timing, making older adults feel sleepy earlier in the evening and wake up earlier in the morning, a pattern often referred to as an “advanced sleep phase.”
Sleep structure also changes with age. Older adults tend to spend less time in deep, restorative stages of sleep and more time in lighter stages. As a result, sleep becomes easier to disrupt, leading to frequent awakenings during the night.
Hormonal changes add to this effect. The body produces less melatonin with age. Melatonin is the hormone that signals it is time to sleep, and lower levels can make it harder to stay asleep or return to sleep after waking. Limited exposure to natural daylight, especially among older adults who spend more time indoors, may further weaken circadian rhythms and worsen sleep quality.
Read also: Melatonin 101: Your Essential Guide to Sleep’s Natural Aid
Health & Medical Factors
Sleep problems in older adults are often closely tied to physical and mental health conditions.
Chronic illnesses such as heart disease, diabetes, and arthritis can cause pain or discomfort that disrupts sleep. Pain and poor sleep often reinforce each other, creating a cycle that becomes harder to break over time.
Night-time urination, also known as nocturia, becomes more common with age and is a frequent cause of sleep interruption. Many older adults wake multiple times a night to use the bathroom, which fragments sleep and reduces overall restfulness.

Certain sleep disorders also become more prevalent with age. These include insomnia, obstructive sleep apnoea, restless legs syndrome, and REM sleep behaviour disorder. Each of these conditions can significantly affect sleep quality and may go undiagnosed if symptoms are mistaken as a “normal” part of ageing.
Medications play an important role as well. Many adults over 65 take multiple prescription or over-the-counter drugs. Some medications can interfere with sleep directly, while others may interact in ways that worsen sleep problems or cause excessive daytime sleepiness.
Lifestyle Changes That Come With Age
Ageing is often accompanied by changes in daily routines and social roles, which can further influence sleep.
Retirement may lead to a less structured day, resulting in irregular sleep and wake times. Lower levels of daytime activity can weaken sleep drive, making it harder to fall asleep at night.
Life transitions such as loss of independence, bereavement, or social isolation can increase stress and anxiety, which may surface as difficulty sleeping. Emotional well-being plays a significant role in sleep quality, especially later in life.

Daytime napping also becomes more common with age. While short naps may be helpful for some, longer or late-afternoon naps can interfere with night-time sleep and contribute to lighter, more fragmented rest.
Sleep Tips for Older Adults
While ageing affects sleep, there are practical steps older adults can take to improve sleep quality.
- Stay physically active: Regular exercise helps older adults fall asleep faster and sleep more soundly.
- Reduce bedroom distractions: Keep televisions, smartphones, and bright lights out of the bedroom.
- Watch what you consume: Limit caffeine, alcohol, smoking, and heavy meals close to bedtime.
- Keep a regular sleep schedule: Go to bed and wake up at the same time each day, including weekends.
- Create a calming bedtime routine: Reading, taking a warm bath, or quiet relaxation can signal the body that it is time to sleep.
Key Takeaways
Changes in sleep are a common part of ageing, but they are not something older adults have to simply accept. Understanding why elderly sleep less highlights the role of biological changes, health conditions, medications, and lifestyle factors in shaping sleep quality.
With the right habits and support, many older adults can improve their sleep and overall well-being. If sleep problems are persistent, disruptive, or affecting daytime functioning, it’s important to seek advice from a healthcare professional for proper evaluation and guidance.
Struggling with your sleep and want clearer answers? Explore our Sleep page for practical guidance, medical insights, and real questions people ask about sleep.
You can also take our Sleep Quiz to see how your sleep habits measure up.
References
National Institute of General Medical Sciences. (2022, March 11). Circadian rhythms. https://www.nigms.nih.gov/education/fact-sheets/Pages/circadian-rhythms.aspx
Li, J., Vitiello, M. V., & Gooneratne, N. S. (2018). Sleep in Normal Aging. Sleep Medicine Clinics, 13(1), 1–11. https://pubmed.ncbi.nlm.nih.gov/29412976/
Miner, B., & Kryger, M. H. (2017). Sleep in the Aging Population. Sleep medicine clinics, 12(1), 31–38. https://pubmed.ncbi.nlm.nih.gov/28159095/
Duffy, J. F., Scheuermaier, K., & Loughlin, K. R. (2016). Age-related sleep disruption and reduction in the circadian rhythm of urine output: Contribution to nocturia? Current Aging Science, 9(1), 34–43. https://pubmed.ncbi.nlm.nih.gov/26632430/