Bariatric and Metabolic Surgery is widely known as a vital and efficient intervention for obesity and related conditions such as diabetes. On World Diabetes Day 14 November, learn how Bariatric and Metabolic surgery can help with not only weight loss, but also with controlling Type 2 Diabetes.
Dr Tan Chun Hai, General Surgeon of Surgicare Bariatric and General Surgery, Gleneagles Hospital, keyhole surgery and bariatric and metabolic surgery specialist, gives in-depth insights on bariatric and metabolic surgery in this article and video.
What is Bariatric And Metabolic Surgery?
The term ‘bariatric’ relates to the treatment of obesity, while the term ‘metabolic’ refers to the treatment of diabetes and other metabolic dysfunctions, which may be correlated with obesity. Bariatric and Metabolic surgery are termed as such as not only is it effective for the treatment of severe obesity, but the resultant weight loss also results in the improvement, prevention and/or resolution of many related diseases such as diabetes, high blood pressure, high cholesterol, obstructive sleep apnea, and many more.
Based on the guidelines issued by the Ministry of Health (MOH) Singapore, patients can be offered bariatric surgery if they have:
- BMI greater than 37.5 kg/m2.
- BMI greater than 32.5 kg/m2 as well as medical conditions related to obesity such as Type 2 Diabetes, OSA etc.
As with any surgery, patients will be evaluated by an experienced team of medical professionals to see if they are suitable to undergo the procedure.
Is Bariatric and Metabolic Surgery Dangerous?
While any surgical procedure has its risks, modern bariatric procedures have strong evidence of not only efficacy but also safety. There are statistics to show that bariatric and metabolic surgery success rates under trained bariatric surgeons are high. Also, it is considered as safe when compared to other elective surgeries such as gallbladder surgeries and total knee replacements! Risk-reduction strategies will be discussed with the patient, to minimize post-operation risks.
When compared to the risks of living with obesity, including obesity-related complications such as diabetes, sleep apnea and cardiovascular events, the risks of bariatric surgery are minimal.
What is the process of Bariatric and Metabolic Surgery?
Pre-operation consultation
Before the operation, the patient will have a consult with their bariatric surgeon. The surgeon will discuss the options and different types of procedures for weight loss, and determine if the patient is a suitable candidate for bariatric and metabolic surgery.
Besides the surgeon, the patient will also meet with multidisciplinary teams as required, such as dietitians, psychologists, cardiologists, respiratory physicians, and endocrinologists. For instance, patients will be evaluated for psychosocial readiness by the psychologist before proceeding to surgery. The dietitian will evaluate the patient for their current nutrition knowledge, and work closely with the patient for nutrition counselling and education.
Operation
Bariatric surgery works by reducing the functioning capacity of the stomach. This reduces the caloric intake of the patient, resulting in weight loss. Besides that, the surgery may also involve reconfiguring parts of the stomach and small intestine, which can alter hormonal signalling to result in effective and sustainable weight loss.
Common bariatric surgery methods incldue Sleeve Gastrectomy and Roux-en-Y (RNY) Gastric Bypass.
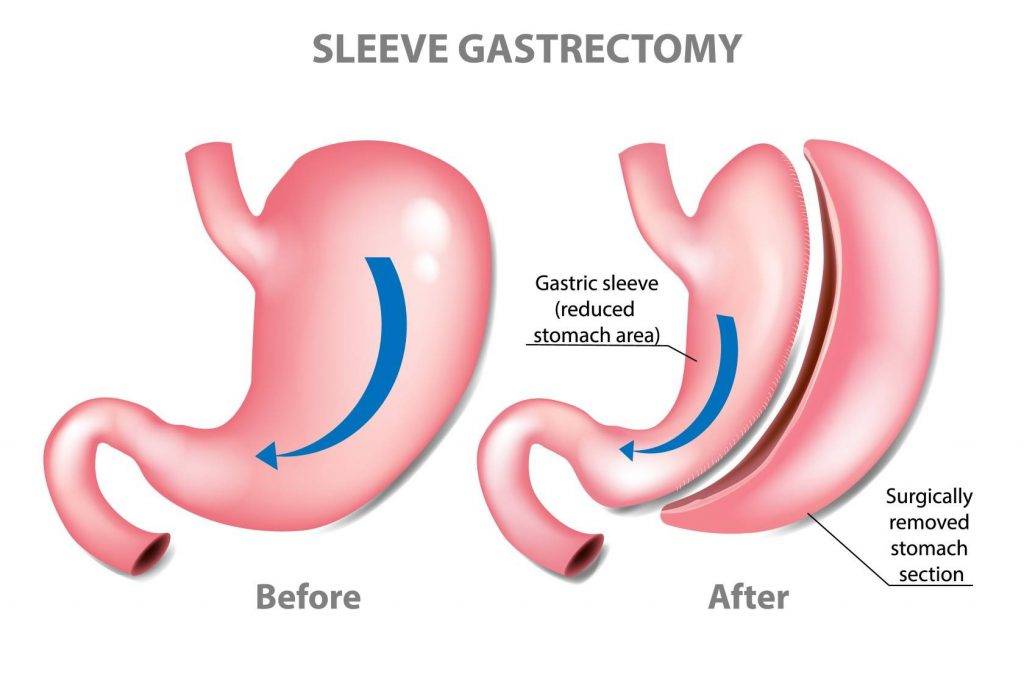
In Sleeve Gastrectomy, approximately 80% of the stomach is removed. The now smaller stomach resembles the size and shape of a banana and holds less food and liquid. This reduces the amount of food (and calories) that can be consumed by the patient. The portion of the stomach removed (gastric fundus) also produces the hormone ghrelin. Ghrelin is known as the hunger hormone, and it facilitates sensations of hunger and fullness. It also has effects on fat storage and blood sugar control. In this way, Sleeve Gastrectomy helps to decrease hunger, increase fullness and support weight loss.
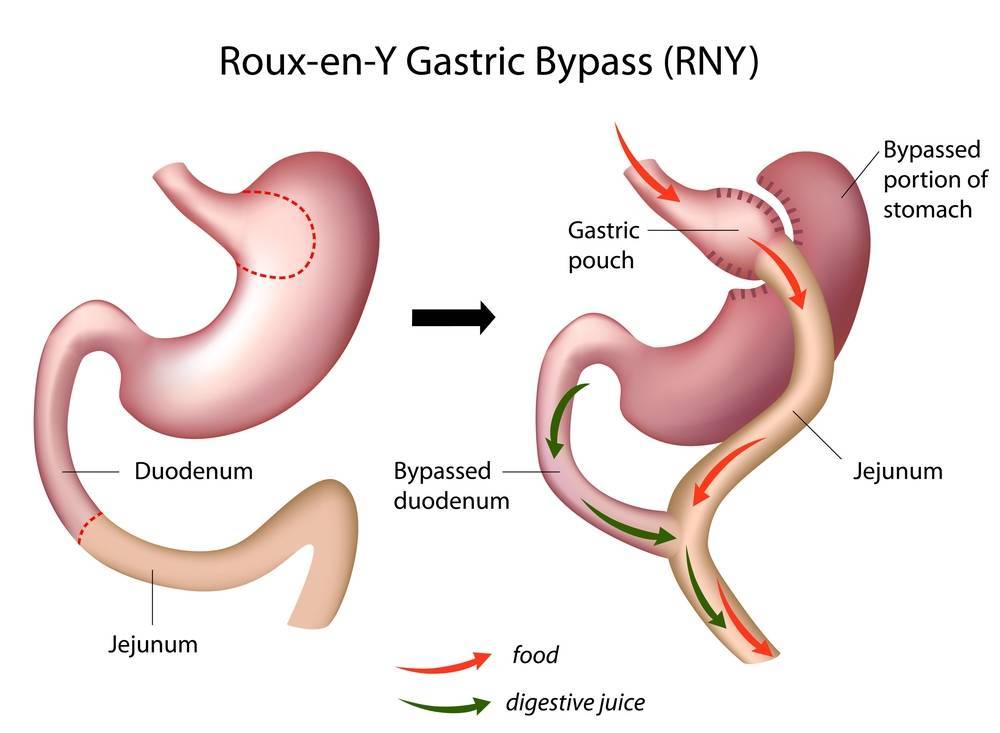
In Roux-en-Y Gastric Bypass, also known as ‘Gastric Bypass’, is another common bariatric surgery method. The stomach is divided into a small pouch and the larger part of the stomach which is bypassed. The small intestine is also divided. The jejunum is connected to the small stomach pouch to allow food to pass through. The duodenum which is attached to the larger stomach also connected back to the small intestine. This results in a bowel connection that resembles the letter Y – its namesake.
With gastric bypass, the stomach pouch is smaller and not able to hold as much food as before, which means fewer calories are ingested. The food also bypasses the larger stomach and the first portion of the small intestine (duodenum), resulting in decreased absorption. This modification has a great effect to decrease hunger, increasing fullness, and supporting weight loss.
Most patients will be admitted on the day of surgery, though some may be admitted a few days before the operation. This will be communicated to you by your bariatric surgeon. There should be no food or drink 8 hours before the scheduled surgery, though plain water is permitted up to 2 hours before the surgery.
The surgery is done via laparoscopic, or keyhole surgery. This means that the bariatric surgeon will access the abdomen via small keyholes instead of large incisions. In comparison to traditional open surgery, keyhole surgery means that the patient will experience:
- Reduced scarring
- Less pain, bleeding and infection risk
- Shorter hospital stay
The duration of surgery depends on the procedure type as well as the complexity of the case and can range from 1-3 hours. Most importantly, the surgery is to be completed safely.
Post-operation
When patients wake up after the surgery, there should be minimal pain that can be controlled by painkillers. They will also have a drip to ensure you have enough fluids during the recovery process. Most patients will be able to get up and go to the toilet within a few hours after the surgery. In fact, it is encouraged to get out of bed as soon as possible after surgery, as it helps to reduce post-operative complications.
In the morning after surgery, a swallow study will be done to rule out any leaks or issues with the surgery. Patients will be placed on a special diet, under the guidance of the dietitian. On top of that, they should take sips of fluid regularly throughout the day to stay hydrated.
Discharge is usually planned one to two days post-surgery. Discharge medication can include painkillers, medication for gastric acid and medication to reduce the risk of gallstones developing. Medication doses for chronic conditions may also be adjusted, reduced or even stopped, and this will be clarified with the patient upon discharge.
Evaluation
After the surgery, it is most important to follow instructions from the surgeon and dietitian and go back for regular evaluation. This is to ensure that the wounds from the surgery and healing well, and that the patient is following the post-operative diet and exercise as planned. Follow-ups will be more frequent after surgery, and they will be spaced further apart as time passes.
What changes can one expect from Bariatric and Metabolic surgery?
Short-term changes
Immediately, patients will be able to feel that they feel full faster from eating a smaller quantity of food. Patients should follow the dietitian and surgeon’s instructions closely to ensure that they are getting enough vitamins and nutrients with the reduced quantity of food ingested.
While every patient is different, one can generally see changes in weight ranging from a decrease of 5-10% within weeks and 10-20% within months of surgery. Over the longer term, more results can be seen.
Long-term changes
Substantial weight loss occurs 18 to 24 months post-surgery. The weight loss may not be linear, and some weight regain may happen years after surgery.
In addition to weight loss, Bariatric and Metabolic surgery can also result in marked improvement in obesity-related conditions, such as:
- Stroke
At 5 years, the risk of ischemic stroke between bariatric surgery and matched controls was 2.8% versus 3.6%. - Cardiovascular events e.g. Heart attack, Heart failure hospitalization
Bariatric surgery is associated with a significantly lower incidence of major adverse cardiovascular events (MACE). - Obesity-related cancers
Bariatric surgery is associated with a significantly lower incidence of 13 obesity-associated cancer and cancer-related mortality.
With weight loss, there are also improvements in the psychological health of patients. This is due to improvements in body image and self-esteem, as well as the sense of control over one’s life. Having a strong support system can help the patient remain positive and motivated throughout the changes brought on by Bariatric and Metabolic surgery, leading to long-term sustainable weight loss.
Conclusion
Surgery is not the magic bullet to cure obesity or metabolic conditions – it is the first step. Take the first step and the bariatric surgeon and their team will be able to walk the weight loss journey with you. It is important to stick to your post-operative bariatric diet under the supervision of the dietitian, make lifestyle changes to increase physical activity, attend regularly scheduled follow-ups with your bariatric surgeon to monitor progress closely, and have a strong support system to help you along your journey.
This article is supported by an educational grant.

