The human pancreas is a solid glandular organ located in the abdomen. It’s about 15 to 20 cm long and 2 to 3 cm wide. The head of the pancreas is surrounded by the first part of small intestine – the duodenum, with the tail of the pancreas covered by the stomach in front. Acute pancreatitis means inflammation of the pancreas that develops quickly.
Normally, the pancreas plays a key role in both digestion and blood glucose regulation. Key enzymes to break down proteins and fats in our food are secreted by the pancreas when food enters the small intestine. Meanwhile, it produces hormones such as insulin and glucagon to keep our blood glucose level within a certain range.
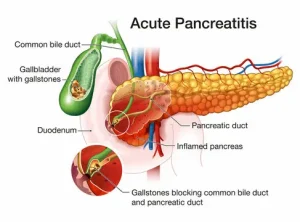
Figure 1. Pancreas
1. What are the symptoms?
Symptoms of acute pancreatitis could come on suddenly and not be specific. Seek medical attention if you have the following symptoms:
- Moderate to severe abdominal pain just below the ribs: it can build up over hours to a few days. This is the most common presentation of patients with acute pancreatitis. However, in rare cases, patients feel no pain at all.
- Pain that radiates to the back
- Nausea and vomiting
- Diarrhoea: when the pancreas can no longer produce digestive enzymes, food would not be properly digested and absorbed.
- Fever
- Swollen abdomen
2. What are the causes?
The most common causes of acute pancreatitis are:
- Gallstones: when gallstones block the tube between the pancreas and small intestine, the pancreas can no longer deliver the digestive juices into the small intestine. The blockage results in self-digestion of the pancreas from the enzyme it produces.
- Heavy alcohol consumption
- Food poisoning: germs in the food can lead to gastroenteritis along with infection of the pancreas
- Infections: both viral and parasite infections are possible causes
- Trauma to pancreas
- Pancreatic cancer: can lead to an acute episode of acute pancreatitis
Meanwhile, like all other diseases, both acute and chronic pancreatitis have genetic factors. People with a family history of pancreatitis are more likely to have episodes of acute pancreatitis in their life span.
3. What are the complications?
Without timely treatment, this condition can lead to serious consequences:
- Kidney failure: acute pancreatitis may cause kidney failure, which has to be treated with dialysis if the kidney failure is severe and persistent.
- Malnutrition: as mentioned above, the pancreas secrets enzymes that are important for nutrient absorption. Disruption of this function leads to minimal nutrient absorption along with weight loss and diarrhoea.
- Diabetes: pancreas regulate blood sugar level using the hormones insulin and glucagon. Diabetes happens when blood sugar levels are above normal.
- Pancreatic cancer: if acute pancreatitis becomes chronic, it is a significant risk factor for developing pancreatic cancer.
4. What are the treatment options?
Treatment options depend on the exact cause of patients’ acute pancreatitis. In general, they would include:
- Pain medications
- Intravenous fluids: diarrhoea and vomiting will result in dehydration. Extra fluids will keep you hydrated.
- Diet management: patients should avoid heavy meat and oily food. Bland food with clear liquid is the best option.
Depending on the cause of acute pancreatitis, patients might need procedures to remove bile duct obstructions from gallstones, pancreatic surgery to drain fluid from the pancreas, treatment for alcohol dependence, etc. Consult your doctors for more information.
