
Heatstroke – On the Rise
With reports about bushfires and melting streetlights in Europe, one cannot forget that Asia is


With reports about bushfires and melting streetlights in Europe, one cannot forget that Asia is

The ketogenic (keto) diet, which involves consuming high amounts of fat, moderate amounts of protein,

Following the tragic death of a six-month-old baby reportedly due to “heatstroke,” the Department of
Systemic lupus erythematosus (SLE) is the most common and serious form of lupus, as discussed in our previous article. It is a chronic autoimmune disorder

A hydrocele is a collection of fluid inside the scrotum of a male. This fluid surrounds the testis and is contained within a lining called tunica vaginalis.

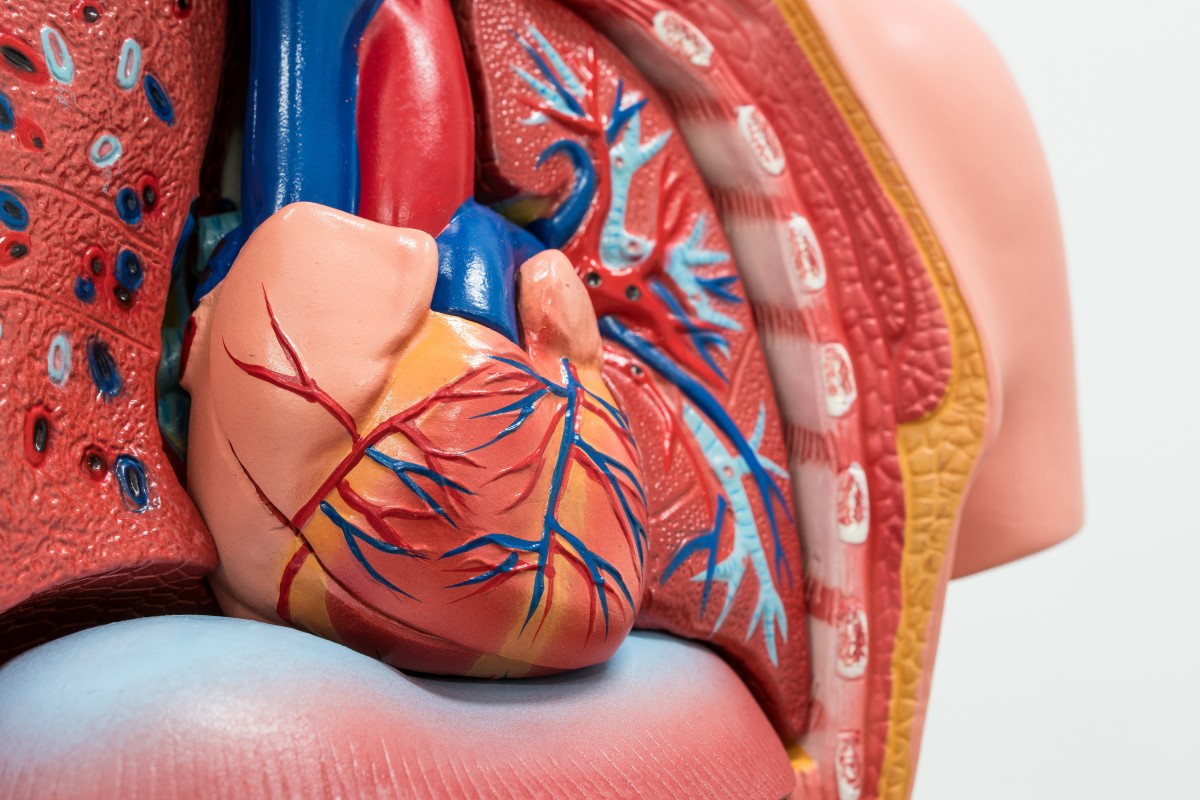
This article first appeared in Orthokinetics Blog. What is cardio? You must have heard of the term cardio (or cardiovascular fitness) being thrown around by




