King Charles III has received medical treatment for an enlarged prostate, a condition common among men his age, Buckingham Palace announced.
The monarch has what is clinically known as benign prostatic hyperplasia (BPH). But what does BPH mean? Dr Ronny Tan and Dr Lie Kwok Ying, Urologists of Advanced Urology Associates, Singapore, help to explain the condition. They also advise on treatment options for this common condition, such as transurethral resection of the prostate (TURP) and prostatic urethral lift (PUL).
Understanding BPH
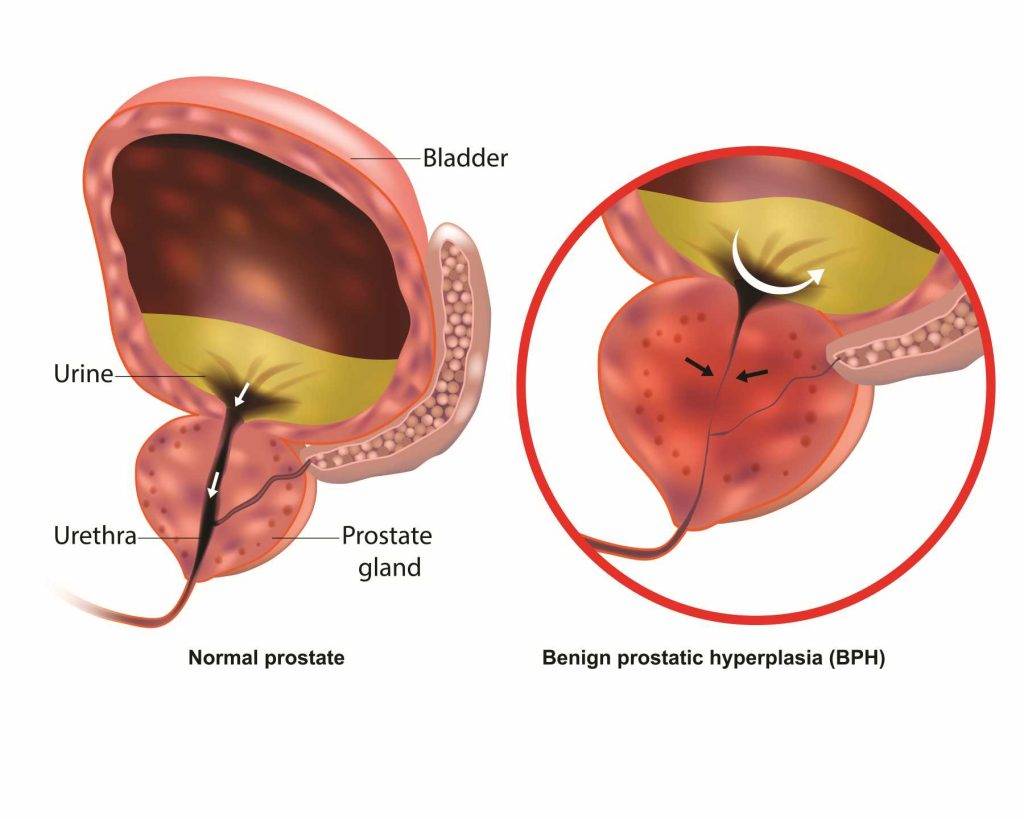
In men, the prostate is a walnut-sized gland that sits between the bladder and the urethra. In benign prostatic hyperplasia (BPH), the prostate is clinically enlarged, obstructing urine flow and other lower urinary tract symptoms (LUTS). BPH becomes more and more common with age – it affects over half of all men when they reach their 50s, to different extents. The older a man gets, the higher the chance he will develop this issue with his prostate gland.
BPH occurs as a part of the natural ageing process in men, akin to menopause in women. Dr Tan explained, “Many men may think that a slow urinary stream is part of ageing and should just go with the flow. However, the truth is the prostate gland may be growing against the flow (pun intended). I would advise any man to seek help from a urologist when there is a disturbance in the (urinary) flow!”
It’s estimated that about 50% of men in their 50s have some form of BPH, and this number can rise to as high as 90% in men over the age of 80.
The King’s Health Condition
The palace stated that the king’s condition was benign and he would attend the hospital for a corrective procedure. King Charles’ public engagements will be postponed for a short recuperation period.
Other Symptoms of BPH
Dr Tan added that lower urinary tract symptoms (LUTS) can be divided into storage symptoms vs voiding symptoms. “Other than slow flow, some men would find themselves having to strain when they pass urine, a sensation of incomplete voiding (urination) and the need to urinate more often during the day and some even at night, affecting their sleep.”
Storage symptoms occur when the bladder is having difficulty storing urine. Storage symptoms include:
- Altered bladder sensation
- Increased daytime frequency
- Increased nighttime urination (Nocturia)
- Urinary urgency
- Urgency incontinence.
Voiding symptoms, on the other hand, occur when there is difficulty passing urine due to obstruction. This can involve:
- Hesitancy
- Intermittency
- Slow flow
- Splitting or spraying of the stream
- Straining
- Dribbling after urination
- Feeling of incomplete bladder emptying
Thankfully, BPH is not considered dangerous in the sense of being life-threatening. However, it can lead to uncomfortable and sometimes serious health issues if not managed properly.
In some cases, BPH can lead to more severe conditions. If left untreated, risks can include:
- Urinary Retention: One of the most serious complications of untreated BPH is acute urinary retention, a sudden inability to urinate. This requires immediate medical attention and might necessitate the insertion of a catheter or emergency surgery.
- Urinary Tract Infections (UTIs): Increased residual urine in the bladder, a consequence of BPH, can lead to frequent urinary tract infections.
- Bladder Damage: Over time, BPH can cause the bladder muscles to weaken and lose the ability to empty the bladder fully, leading to chronic urinary retention and other bladder problems.
- Kidney Damage: In severe cases, the blockage of urine flow can lead to kidney damage or infection.
- Bladder Stones: These are small minerals that form in the bladder due to an inability to empty the bladder fully. They can cause infection, bladder irritation, blood in the urine, and obstruction of urine flow.
- Decreased Quality of Life: The symptoms of BPH, such as frequent urination, nocturia (frequent urination at night), and a weak urine stream, can affect sleep patterns and daily activities, leading to a decreased quality of life.
- Increased Risk of Falls: For older adults, especially, nocturia increases the risk of nighttime falls, which can lead to serious injuries.
Therefore, it is important to get screened for the condition and seek treatment if needed.
If you think you might have BPH, take the International Prostate Symptom Score (IPSS) self-assessment here: https://bphsolution.com/sg/ipss-questionnaire/. It is a useful, 8-question quiz to help you assess your symptoms and help facilitate conversations with your urologist when it comes to managing your condition.
Treatment Options for Enlarged Prostate
If symptoms of BPH become severe, patients may require medical treatments and sometimes surgery. Common medications include alpha blockers and 5-alpha-reductase inhibitors, which relax the prostate or inhibit hormonal changes causing the enlargement.
Surgery may be necessary if the condition progresses, as in King Charles’s case. Buckingham Palace did not specify the exact procedure. However, experts suggest that a transurethral resection of the prostate (TURP) was likely used. This surgery involves scraping the inside of the prostate gland to relieve pressure on the urethra.
Dr Lie also shared that in Singapore, “the late Prime Minister Mr Lee Kuan Yew underwent a transurethral resection of prostate (TURP) in 2003. TURP has been and is still the traditional gold-standard treatment, but a lot of times, newer procedures can match or beat that effectiveness with fewer side effects and fewer problems.”
Dr Tan added that there are newer minimally invasive surgical techniques such as “UroLift (prostatic urethral lift).” In a Prostatic Urethral Lift (PUL) procedure, (A) The device is introduced to the enlarged prostate, under cystoscopic guidance; (B) the lobes of the prostate are compressed by the device and a tiny implant is deployed. (C) Additional implants are delivered by the surgeon depending on the patient’s condition, to achieve the final result of (D) a widened and unobstructed channel for urine.
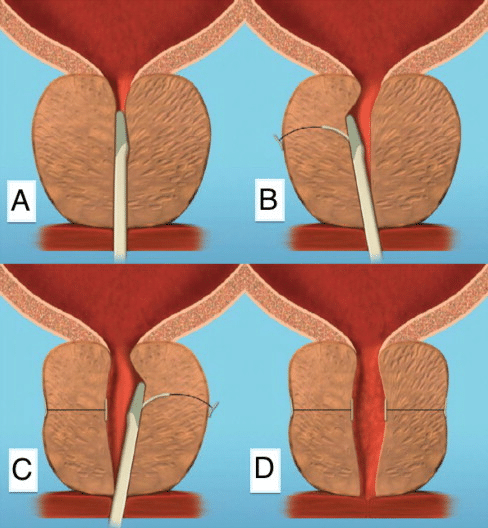
Source: Garcia C, Chin P, Rashid P, Woo HH. Prostatic urethral lift: A minimally invasive treatment for benign prostatic hyperplasia. Prostate Int. 2015;3(1):1-5. doi:10.1016/j.prnil.2015.02.002
“These techniques would not have any sexual dysfunction compared to TURP.” He added. Studies have shown PUL to be a well-tolerated procedure, that producing improvement in urinary symptoms and function while at the same time preserving patients’ sexual function. In comparison, TURP is often associated with sexual complications such as ejaculatory failure, retrograde ejaculation and decreased ejaculate volume.
Implications of the King’s Treatment
The king’s decision to publicise his condition is seen as a move to destigmatise health issues among men and encourage proactive health management. His treatment also sheds light on the advancements in medical science, offering practical solutions for conditions like BPH.
Conclusion
King Charles’s treatment for an enlarged prostate serves as a reminder of the importance of men’s health issues, particularly those associated with ageing. It underscores the need for awareness and timely medical intervention in managing conditions like BPH, which can significantly impact quality of life.
As medical technology advances, treatments become more effective and less invasive, offering hope and improved health outcomes for millions of men worldwide. Therefore, men above 50 need to be checked for this condition. The International Prostate Symptom Score (IPSS) is a simple, validated questionnaire one can try at home to check the severity of one’s symptoms. Try the self-assessment quiz at https://bphsolution.com/sg/ipss-questionnaire/ and discuss your results with a trusted healthcare professional.
Dr Ronny Tan is a Specialist Urologist and Andrologist. Dr Lie Kwok Ying is a Senior Consultant Urologist. Both doctors are based in Advanced Urology Associates, Singapore.
This article is supported by an educational grant.
References:
-
Lim YW, Tay KJ, Ho HSS. The Minimally Invasive Treatments for Benign Prostrate Hyperplasia. Proceedings of Singapore Healthcare. 2014;23(1):65-73. doi:10.1177/201010581402300111
-
Singapore Urological Association Male Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia Guidelines Committee 2015. Singapore Urological Association Clinical Guidelines for Male Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia [published correction appears in Singapore Med J. 2018 Jun;59(6):338]. Singapore Med J. 2017;58(8):473-480. doi:10.11622/smedj.2017082
-
Gacci M, Sebastianelli A, Spatafora P, et al. Best practice in the management of storage symptoms in male lower urinary tract symptoms: a review of the evidence base. Ther Adv Urol. 2017;10(2):79-92. Published 2017 Dec 7. doi:10.1177/1756287217742837
-
Kramer G, Mitteregger D, Marberger M. Is Benign Prostatic Hyperplasia (BPH) an Immune Inflammatory Disease? European Urology. 2007; 51(5):1202-1216. doi:10.1016/j.eururo.2006.12.011
-
Braeckman J, Denis L. Management of BPH then 2000 and now 2016 – From BPH to BPO. Asian J Urol. 2017;4(3):138-147. doi:10.1016/j.ajur.2017.02.002
-
Garcia C, Chin P, Rashid P, Woo HH. Prostatic urethral lift: A minimally invasive treatment for benign prostatic hyperplasia. Prostate Int. 2015;3(1):1-5. doi:10.1016/j.prnil.2015.02.002
-
Perera M, Roberts MJ, Doi SA, Bolton D. Prostatic urethral lift improves urinary symptoms and flow while preserving sexual function for men with benign prostatic hyperplasia: a systematic review and meta-analysis. Eur Urol. 2015;67(4):704-713. doi:10.1016/j.eururo.2014.10.031
-
Al Demour SH, Abuhamad M, Santarisi AN, et al. The Effect of Transurethral Resection of the Prostate on Erectile and Ejaculatory Functions in Patients with Benign Prostatic Hyperplasia. Urol Int. 2022;106(10):997-1004. doi:10.1159/000524957













