Osteopenia is a condition where there is low bone mass, indicating weaker bones more prone to breakage, but not as severe as osteoporosis. Bone mass can keep growing and peak bone mass is usually achieved around 25 to 30 years old. After peak bone mass is reached, the body loses bone mass faster than it builds new bone, especially with ageing. Although everyone will lose bone with age, people who developed a higher peak bone mass when young are better protected against osteopenia, progression to osteoporosis and related fractures later in life.
World Osteoporosis Day falls on 20 October this year. In conjunction with it, let’s look at osteopenia, one of the condition that often precludes osteoporosis.
What causes osteopenia?
Failure to reach peak bone mass in adulthood, due to:
- Certain diseases which prevent calcium from being absorbed into the bones, e.g. celiac disease, inflammatory bowel disease
- Inadequate nutrition (calcium, vitamin D), hormonal imbalances and reduced body weight due to eating disorders like anorexia and bulimia
- Genetic predisposition to osteoporosis; environmental factors only account for 20% of peak bone mass
- Medications e.g. long-term use of anticonvulsants, corticosteroids
- Lifestyle habits, such as smoking or drinking too much alcohol
Accelerated loss of bone, due to:
- Above-mentioned factors
- Hyperthyroidism
- Decline in oestrogen levels from postmenopausal state or surgical removal of ovaries
Other natural risk factors predisposing to Osteopenia include:
- Being Caucasian or Asian
- Female gender: women have lower bone density than men in general
Symptoms of osteopenia
As bones weaken gradually, and deterioration is not painful, most osteopenic people are asymptomatic. They do not find out that they have low bone density until a bone fracture with consequent pain occurs. One more apparent tell-tale sign of bone loss is a decrease in >1 inch of height in old age.
Diagnosis
Bone mineral density (BMD) is a marker for the strength of bone and determines the risk of breakage. This can be measured using a non-invasive and low energy x-ray test called the dual-energy x-ray absorptiometry (DEXA) scan that measures the mineral content of the bone, usually in the lumbar spine, hips and wrists. DEXA scores are reported as “T-scores” and “Z-scores”.
T-scores
The T-score is a standard deviation which shows how much your bone mass differs from the bone mass of an average healthy 30-year-old adult. The lower the score, the more porous the bone and the higher the risk of bone breakage.
Osteopenia is defined by the World Health Organisation (WHO) as a T-score between –1.0 and –2.5 standard deviations below normal i.e. bone mass that is 10% to 25% below an average healthy 30-year-old adult.
Osteoporosis is defined by the WHO as a T-score lower than -2.5 or 2½ standard deviations below normal i.e. bone mass that is 25% lower than the average healthy 30-year-old.
If your bone density results classify you to have osteopenia, a BMD test will be scheduled for monitoring every two to four years.
Z-scores
The Z-score is a standard deviation which shows how much your bone mass differs from the bone mass of an average adult of the same age and gender. A Z-score is helpful in diagnosing secondary osteoporosis and is always used for children, young adults, women who are pre-menopausal, and men under age 50.
If you have a very low Z-score (≥-2), it your doctor may order additional blood tests to determine if there are other factors that may be causing lower than expected bone density e.g. kidney disease, parathyroid gland dysfunction.
Treatment and Prevention
Osteopenic patients have a lower fracture risk than those with osteoporosis and the goal of treatment is usually to prevent progression to osteoporosis.
Bones will weaken as we age but there are preventive measures to delay deterioration:
- Regular exercise (~30 minutes daily) that includes:
- Weight-bearing exercise (e.g. walking, jogging)
- Exercises to improve balance and muscle strength (e.g. swimming, cycling, hip abductors, prone leg lifts, toe and heel raises)
- Eating foods rich in calcium (e.g. dairy products, spinach, broccoli) and Vitamin D (e.g. eggs, oily fish like salmon); some cereals and orange juices are fortified with both
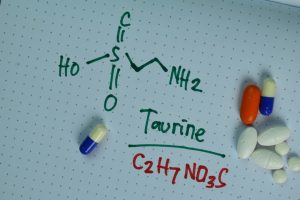
- Taking Calcium and/or Vitamin D supplement, especially those on restrictive diets e.g. vegans
- Regular sun exposure helps in synthesis of Vitamin D i.e. ~ 5 to 30 minutes of midday sun exposure twice a week on the face, arms, neck, or back (darker-skinned people may need a longer time)
- Stop smoking
- Avoid drinking excessive amounts of alcohol
- Avoid excessive caffeinated beverages (coffee, tea, energy drinks, soda); the FDA recommends 400 mg of caffeine per day (~4 cups of coffee) as a generally safe amount
- Taking measures to prevent falls and bone injury, especially for the elderly
- Installing grab-bars in the bathroom at home
- Place non-slip mats in the bathroom
- Ensure proper lighting/night-lights
- Wear non-slip socks
Medications are usually prescribed only if the BMD is close to osteoporosis level or if a patient is found to be at high risk for fractures The Fracture Risk Assessment Tool (FRAX) score calculates the risk of having an osteoporosis-related fracture in the next 10 years; a high FRAX score may sometimes necessitate pharmacological treatment. Some examples of medications used include antiresorptive agents like bisphosphonates (e.g. risedronate, alendronate), denosumab, or bone formation-stimulating drugs such as teriparatide or abaloparatide.
Conclusion
Adopting healthy habits (adequate nutrition and active lifestyle) can help improve bone density and delay progression to osteopenia and osteoporosis.